Case Study: Left Knee arthrotomy and implantation of
cultured autologous chondrocytes on porcine membrane
(MACI) in a 47 year-old patient
The surgical investigation of a joint known as an arthrotomy entails looking at the ligaments, cartilage, and intra-articular structures. In a process known as matrix-induced autologous chondrocyte implantation, or MACI, a patient’s own cells are utilized to help the knee joint regenerate new cartilage.
A 47 year-old patient visited our office with complaints regarding left knee pain. She works as a hemodialysis nurse at SBU and is out of work due to this pain. She is having pain, swelling, and buckling.
Swelling has decreased. MRI were reviewed and discussed wherein the results have shown 9 x 6 mm full-thickness chondral defect in the midportion of the medial femoral condyle. Focal area of Chondral fissuring and partial-thickness cartilage loss in the central trochlea. Intact medial and lateral meniscus.
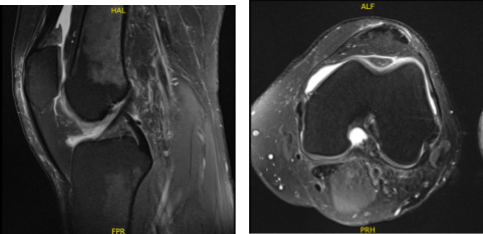
MRI-3T Left knee non-contrast
We discussed treatment options and the patient opted for surgical management. The patient was leaning towards possible repair and reconstruction of the osteochondral defects in an attempt to make it somewhat longer and avoid knee arthritis and early knee replacement.
We discussed chondroplasty vs. osteochondral bone grafting vs. joint replacement surgery in the possible future. The patient understood and agreed for arthroscopic chondroplasty and measurements.
We discussed the risks and benefits including infection, bleeding, injury to the nerves and vessels, possible numbness, need for repeat surgery in case we need to do a repair or reconstruction, arthritis, rehabilitation, need in the surgery in the future, among others.
We also discussed the complications including blood clot, femoral artery complications or death. The patient understood and signed the informed consent.
The patient was taken to the operating room and she was placed on the right sided operating room table. 10 cc of 2% Lidocaine mixed with .5% Marcaine without epinephrine was injected into the mid portal. A total injection of 30 cc was injected into the left knee. Sedation was given to the patient.
The left knee was prepped and draped aseptically in the usual sterile fashion. Compression was applied. The knee was put in a clamp. Preoperative consent was given already. The tourniquet was elevated to 250 mmHg.
After exsanguination an incision was made. The lateral portal anesthesia was given. A medial anterior portal incision was made with the use of a spinal needle. There was arthritis along the medial femoral condyle and medial tibial plateau. The meniscus was intact.
There was a Grade IV defect of the medial femoral condyle which was debrided with the use of curette and debrided, and abrasion chondroplasty was performed with the use of a curette. The defect was measured and was 1.5 cm by 1.5 cm. Examination revealed an intact ACL.
The examination noted lateral tibial tendon patellofemoral compartment showed intact cartilage. Examination of the patellofemoral compartment showed intact cartilage over the patella but there was Grade III to Grade IV osteochondral lesion of the trochlea.
Debridement of this lesion was performed to stable margins. The defect was measured to be 1.5 cm x 1 cm. All the measurements were taken. All the pictures were taken and saved.
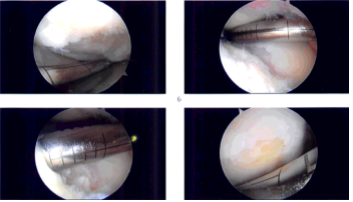
Intraoperative Arthroscopy Images
The knee was drained. Closure was done with 3-0 nylon. Dressing was done with the use of Xeroform, double 4 x 8, Ace wrap, the tourniquet was deflated. The patient was extubated and brought to the recovery room in stable condition.
She was in status post arthroscopic surgery left knee chondroplasty, measurements of the osteochondral defect left knee in preparation for possible procedure in the future. Excisional biopsy of cartilage from the suprapatellar notch.
We discussed treatment options in the postop period and the patient opted for autologous cultured chondrocyte implantation. The chondrocyte cultures were prepared in the lab on a porcine membrane and the patient was posted for surgery
. We discussed other treatment options as well as risks and complications including infection, bleeding, injury to adjacent nerves and vessels, failure, arthritis, need for total knee replacement, rehabilitation among others.
We also discussed risks and complications including blood clots, cardiac, pulmonary, neurological complications including death. The patient understood and signed the informed consent.
The patient was taken to the operating room where she was placed on a well-padded operating table. General anesthesia was induced in the form of LMA. Left lower extremity was prepped and draped aseptically in a usual fashion with a bump under the head and a lateral post. Preop antibiotic was given. Tourniquet was not inflated for the procedure.
Incision was planned along the midline anterior to the patella. It was extended from the distal quadriceps to the tibial tuberosity. Deep dissection and flap was raised above the patellar retinaculum as well as the patella.
A medial parapatellar arthrotomy was done with the use of a sharp blade taking precautions not to injure the cartilage as well as the meniscus. Once the arthrotomy was performed, a good exposure could be obtained for the medial femoral condyle and the patient’s knee was in 90-degree flexion and off the trochlea when the knee was in extension.
The lesions were again seen. In preparation for the transplant, oval template was used for the medial femoral condyle with the knee in 90-degree flexion. The cartilage along the oval template was cut with the use of a blade followed by curette to reach a stable subchondral region.
There was some extension of the loose cartilage posteriorly, which was also excised in line with the defect. Templating of the defect was done with the use of the cover of chromic catgut. Once a good templating was done, it was taken to the back table.
The MACI autologous cultured chondrocytes on the porcine membrane were opened and dropped on the operating field and the template was used to cut the MACI with the cells facing up. Once the template was cut, the medial femoral condyle was checked for any active bleeding.
Hemostasis was achieved well. Two drops of Vistaseal were put on the floor and the graft MACI was put on it with the cells facing towards the bone. The Tegaderm was removed and the MACI membrane was patted well with the use of patty gently.
Three minutes were given to dry. Vistaseal was applied along the margins also. The posterior margin of the membrane was sutured to the adjacent cartilage using 6-0 Vicryl. Once it was implanted well and dried, the knee was extended to focus attention on the trochlear lesion.
An oval cutting block was again taken, small size, and put on the defect and punched enough to make an abrasion along the cartilage. Knife and curette were used to create the defect. Subchondral bone was reached. Hemostasis was induced with the use of Gelfoam-soaked thrombins.
The MACI membrane was cut with the use of the same cutting block and hammer. The cut was made with a piece of tourniquet behind it. Now the cell surface facing the bone membrane was put onto the defect after application of Vistaseal.
It was allowed to dry for 3 minutes followed by application of Vistaseal on the edge and again allowed to dry for 3 minutes. Once it was dried, the knee was ranged gently and the grafts were checked on both sides and found to be stable.
Knee was gently irrigated with the use of normal saline. Hemostasis was achieved and closure was done in layers using PDS 4 and 2-0 Vicryl for the arthrotomy followed by 2-0 Vicryl for subcutaneous and 3-0 Monocryl for the skin.
Dressing was done with the use of Xeroform, 4x 8’s, ABD, Webril, Ace wrap. Knee immobilizer was applied. The patient was given a post op femoral block. The patient was extubated and went to recover in a stable condition.
The patient was seen for post operative check up. We have decided to do formal physical therapy as well as a home exercise program for rehabilitation of the knee.
Patients regularly followed an office visit every 3-4 weeks. Patient did well after the surgery and continued physical therapy. Patient checked in for a follow up visit after a month and saw significant improvement on her knee.
Disclaimer – Patient’s name, age, sex, dates, events have been changed or modified to protect patient privacy.

Dr. Vedant Vaksha
I am Vedant Vaksha, Fellowship trained Spine, Sports and Arthroscopic Surgeon at Complete Orthopedics. I take care of patients with ailments of the neck, back, shoulder, knee, elbow and ankle. I personally approve this content and have written most of it myself.
Please take a look at my profile page and don't hesitate to come in and talk.
