Transient Osteoporosis of the Hip
The transient osteoporosis of the hip joint is the temporary loss of bone density in the head of the femur. The condition is often self-limiting and is different from both age-related osteoporosis and avascular necrosis of the hip joint.
The transient osteoporosis of the hip joint may cause disabling pain in the hip region that may cause the patient to limp. The management is nonsurgical but it is important to rule out other serious bone diseases such as avascular necrosis that may require early surgery.
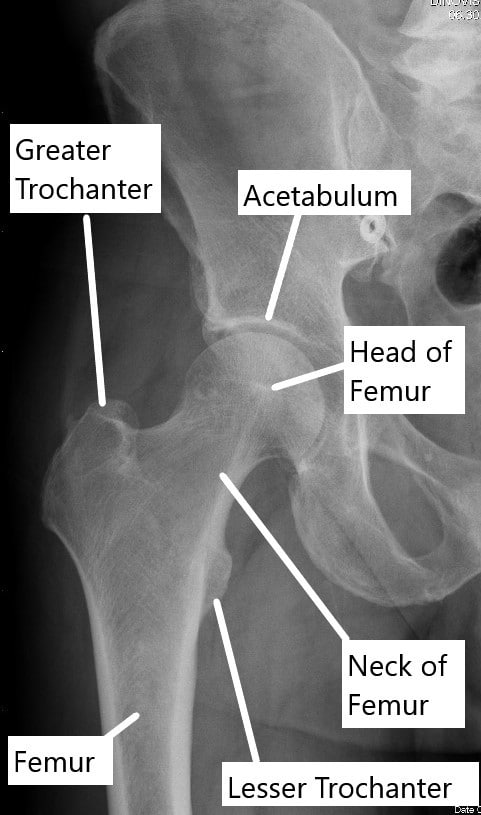
X-ray showing normal anatomy of the hip joint.
The bones in the human body are living tissues that require a constant supply of nutrients and oxygen to maintain function. The bones consist of a bony matrix that is mineralized with calcium and phosphate to provide strength. The bone cells are involved in the constant turnover of the mineralization to maintain the structure and strength of the bone.
The hip joint is formed by the head of the femur that rotates in the socket formed by the acetabulum. The ends of the ball and the socket are covered with a glistening white tissue known as the articular cartilage. The articular cartilage allows the smooth rotation of the joint. The hip joint is unique due to its limited blood supply.
Transient Osteoporosis of the Hip joint – Causes and Risks
The exact cause of transient osteoporosis of the hip joint is unknown but it has been hypothesized to be caused by temporary disruption of the blood supply of the head of the femur. The loss of blood supply may be caused by blockage of the veins of the head of the femur. The veins take the blood away from the head of the femur after the nutrients are extracted from the arteries.
The blockage of the veins may create a back pressure that may lead to swelling in the head of the femur. The swelling may further reduce the blood supply to the head of the femur. The density of the head of the femur reduces leading to specific signs in radiological studies. The reduction in the bone density (osteolysis and osteoporosis) may decline further over the months and slowly recover in about 12 months.
The transient osteoporosis of the hip occurs most often in middle-aged men and pregnant females in the last 3 months of their pregnancy.
Symptoms
Patients with transient osteoporosis of the hip joint often complain of hip pain located over the groin region. The pain may be located on the side of the hip or even in the buttock besides the groin. Patients report worsening of the pain on weight-bearing activities such as walking, navigating stairs, or standing.
The hip pain may significantly worsen to the point where the patient may start limping. The limping occurs as the patient tries to spend less time on the painful hip while walking. The patient may also have painful movements, especially when doing those movements by themself (active movements). As the head of the femur gets considerably weaker, any high-impact activity may potentially lead to a fracture of the bone.
Diagnosis
The diagnosis of transient osteoporosis of the hip joint is a diagnosis of exclusion after all other possible diseases have been ruled out. The physician performs an extensive physical examination to look for tenderness (points of pain) and the hip range of motion. The physician may request radiological studies in the form of an X-ray.
The initial X-rays of the hip joint may be normal and only later X-rays may show a decrease in density of the hip joint. The joint space is always maintained (normal) in transient osteoporosis of the hip joint.
The physician may also order a CT scan that shows a higher resolution of the bony structures in the hip joint. MRI may show the early changes associated with transient osteoporosis of the hip. The MRI scan of the hip joint may show bone edema and the loss of density. A nuclear bone scan similarly is able to pick up the changes associated with transient osteoporosis earlier as compared to other modalities.
The radiological studies may be withheld in a pregnant female although an MRI is considered safe in pregnancy. However, any imaging study in a pregnant female is only done after consultation with their obstetrician and their primary care provider.
Management
The treatment of transient osteoporosis of the hip joint is nonsurgical. The management involves the use of pain medication such as nonsteroidal anti-inflammatory drugs like ibuprofen or naproxen, partial weight-bearing, and avoidance of any high impact activity. The patients may be advised to use a cane to offload the joint. Physical therapy is aimed to maintain the strength and flexibility of the muscles around the hip while not bearing weight.
Prognosis and Differential Diagnosis
The patients report a complete resolution from their symptoms in one to one and a half years. There is no residual deformity of disease that may cause long-term disability.
Transient osteoporosis may be confused with generalized age-related osteoporosis that affects all the bones of the body and not just the head of the femur. The patients suffering from osteoporosis are usually post-menopausal females or patients with metabolic bone disorders.
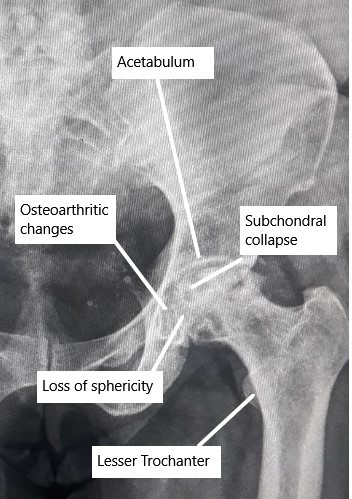
X-ray showing advanced AVN changes in the Hip.
Transient osteoporosis may also be mistaken with another bone disease called avascular necrosis (AVN). In AVN of the hip joint, there is bone death of the head of the femur secondary to disruption of the blood supply. The exact cause is unknown in AVN but patients with a history of corticosteroid use or alcohol abuse are more susceptible to having AVN.
Any injury to the hip that may disrupt the blood supply may also cause AVN. Compared to transient osteoporosis, AVN of the hip generally affects both the hip joints. AVN of the hip joint is a progressive disorder that may require early surgical intervention compared to transient osteoporosis that is managed nonsurgically.
Do you have more questions?
Is transient osteoporosis of the hip a common condition?
Transient osteoporosis of the hip is considered rare but can occur, particularly in certain demographics such as middle-aged men or pregnant women.
What causes transient osteoporosis of the hip?
The exact cause of transient osteoporosis of the hip is unknown, but it is believed to involve factors such as hormonal changes, reduced blood flow to the hip joint, and mechanical stress.
How is transient osteoporosis of the hip diagnosed?
Diagnosis typically involves a combination of clinical evaluation, imaging studies such as X-rays, MRI scans, and bone density tests, and ruling out other possible causes of hip pain.
What are the risk factors for developing transient osteoporosis of the hip?
Risk factors may include being male, middle-aged, or pregnant, as well as certain medical conditions such as hyperparathyroidism or corticosteroid use.
Can transient osteoporosis of the hip affect both hips simultaneously?
Yes, transient osteoporosis of the hip can affect both hips simultaneously, although it may initially present in one hip before involving the other.
Is transient osteoporosis of the hip associated with any complications or long-term effects?
In most cases, transient osteoporosis of the hip resolves on its own with appropriate management and does not lead to long-term complications. However, in some instances, it may progress to avascular necrosis of the hip joint.
What are the treatment options for transient osteoporosis of the hip?
Treatment typically focuses on pain management, reducing weight-bearing activities on the affected hip, physical therapy to maintain joint mobility and muscle strength, and, in some cases, medications to improve bone density.
How long does transient osteoporosis of the hip typically last?
Transient osteoporosis of the hip usually resolves spontaneously within a few months, although the duration can vary depending on individual factors and the severity of the condition.
Can transient osteoporosis of the hip recur after resolution?
While rare, transient osteoporosis of the hip can recur in some individuals, particularly if underlying risk factors persist or if there is inadequate management of the condition.
Are there any lifestyle modifications or precautions recommended for individuals with transient osteoporosis of the hip?
Yes, individuals with transient osteoporosis of the hip may be advised to avoid activities that exacerbate hip pain or increase stress on the joint, maintain a healthy weight, and ensure adequate intake of calcium and vitamin D to support bone health.
Can transient osteoporosis of the hip lead to permanent damage or disability?
In most cases, transient osteoporosis of the hip does not lead to permanent damage or disability if managed appropriately. However, in rare instances or severe cases, it may progress to avascular necrosis or other complications.
Are there any surgical interventions available for treating transient osteoporosis of the hip?
Surgical interventions are typically not necessary for transient osteoporosis of the hip, as the condition usually resolves with conservative management. However, in cases of severe pain or complications such as fracture, surgical options may be considered.
Can physical therapy or rehabilitation exercises worsen symptoms of transient osteoporosis of the hip?
Physical therapy and rehabilitation exercises are generally beneficial for maintaining joint mobility and muscle strength in transient osteoporosis of the hip, but it’s essential to avoid activities that exacerbate pain or discomfort.
Are there any alternative or complementary therapies that may help manage symptoms of transient osteoporosis of the hip?
While not a replacement for conventional medical treatment, some individuals may find relief from symptoms of transient osteoporosis of the hip through therapies such as acupuncture, chiropractic care, or herbal supplements. However, the effectiveness of these approaches varies, and consultation with a healthcare provider is recommended.
Can transient osteoporosis of the hip affect other joints in the body besides the hips?
While transient osteoporosis of the hip primarily affects the hip joints, it can theoretically affect other weight-bearing joints such as the knees or ankles, although this is less common.
Are there any specific precautions or considerations for pregnant women with transient osteoporosis of the hip?
Pregnant women with transient osteoporosis of the hip may require specialized management to ensure optimal pain relief and mobility while considering the safety of treatment options for both the mother and the fetus.
Can transient osteoporosis of the hip cause permanent changes in bone density or structure?
In most cases, transient osteoporosis of the hip does not cause permanent changes in bone density or structure, as it is a self-limiting condition that typically resolves without long-term effects.
How can I prevent transient osteoporosis of the hip from recurring in the future?
Preventing recurrence of transient osteoporosis of the hip may involve addressing underlying risk factors such as hormonal imbalances, avoiding excessive weight-bearing activities, maintaining a healthy lifestyle, and following any recommendations from healthcare providers for bone health maintenance.
Are there any specific medications or supplements that can help prevent or treat transient osteoporosis of the hip?
In some cases, medications such as bisphosphonates or calcitonin may be prescribed to improve bone density and reduce the risk of fracture in transient osteoporosis of the hip. Additionally, calcium and vitamin D supplements may be recommended to support bone health.

Dr. Suhirad Khokhar
My name is Dr. Suhirad Khokhar, and am an orthopaedic surgeon. I completed my MBBS (Bachelor of Medicine & Bachelor of Surgery) at Govt. Medical College, Patiala, India.
I specialize in musculoskeletal disorders and their management, and have personally approved of and written this content.
My profile page has all of my educational information, work experience, and all the pages on this site that I've contributed to.
