Case Study: Management of the 52-year-old Female
with Rotator Cuff Tear and Glenohumeral Arthritis
The patient is a 52-year-old female who presents to our office with complaints of worsening left shoulder pain and weakness for the past year. The patient reports an injury to the left shoulder in a motor vehicle accident. The patient did not seek medical attention at the time of the injury.
The patient describes the pain as severe in intensity and sharp in character. The pain is particularly bothersome at night and wakes her up from her sleep. The patient states NSAIDs help in decreasing the intensity of pain but lately, the medications have been ineffective.
The left shoulder pain is not associated with swelling, bruising, numbness, tingling, radiating pain, weakness, bowel or bladder abnormality, gait problem, or limping, giving way, hand function difficulty. According to the patient activities such as walking, lifting, exercise, kneeling, making the symptoms worse.
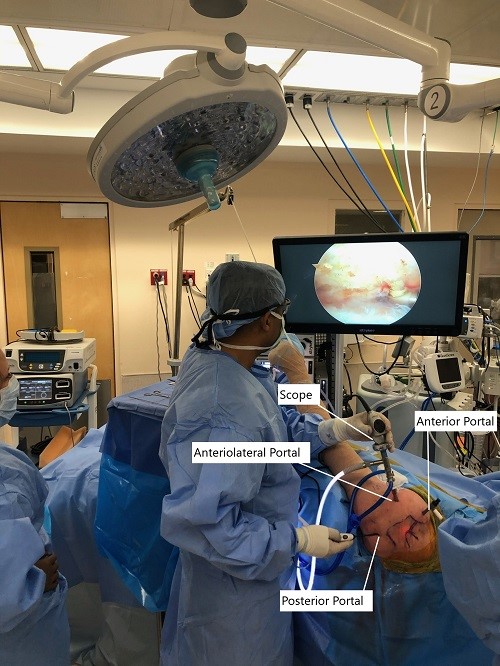
Intraoperative picture of arthroscopic shoulder surgery set up.
The patient previously had cortisone injections in the left shoulder and the injections provided relief only for a few weeks. The patient also received physical therapy but had minimal relief from symptoms. The medical history of the patient is unremarkable and she has previously undergone surgery in the form of a caesarian section and left shoulder rotator cuff repair (arthroscopic). She denies smoking or the use of any illicit drugs. She is currently not working.
On physical examination, there are visible scars from the prior arthroscopic surgery. There is tenderness to palpation on the subacromial bursa and bicipital groove. Active range of motion of the left shoulder – external rotation 40 deg, forward flexion 80 deg, extension 20 deg, and abduction 80 deg. Hawkins test, Neer’s test, and empty can sign were positive. The examination of the right shoulder and the cervical spine was normal.
MRI study of the left shoulder suggested a rotator cuff tear. Various treatment options were discussed at length with the patient and she opted for surgical management.
The risks, benefits, complications of surgical treatment including infection, bleeding, nonhealing, need for repeat surgery, need for shoulder arthroplasty in future, injury to adjacent nerves and vessels, rehabilitation, systemic complications including blood clot, cardiac, neurological, pulmonary complications including death were discussed at length with the procedure. The patient understood and signed the informed consent.
PREOPERATIVE DIAGNOSIS: Rotator cuff tear of the left shoulder.
POSTOPERATIVE DIAGNOSES:
- Rotator cuff tear of the left shoulder.
- Acromial spur.
- Grade 3 to grade 4 osteoarthritis of the glenohumeral joint.
- Synovitis of the glenohumeral joint.
OPERATIONS:
- Left shoulder arthroscopic rotator cuff repair.
- Left shoulder arthroscopic acromioplasty.
- Left shoulder arthroscopic limited debridement of the glenohumeral joint.
DESCRIPTION OF PROCEDURE: The patient was taken to the operating room where she was placed on a well-padded operating table. General anesthesia was induced. A supraclavicular block was given preoperatively. The patient was turned into the right lateral position with the left shoulder up. He was held in an excellent position in the beanbag. The axillary roll was used to pad the axilla. All the bony prominences were well padded.
The left upper extremity was prepped and draped aseptically in the usual fashion. Preoperative antibiotics were given. A posterolateral entry portal was made. The scope was entered. Examination of the glenohumeral joint showed extensive synovitis, degenerative arthritis of the glenohumeral joint more on the humeral head, absence of biceps, and the rotator cuff tear in the region of the supraspinatus and in infraspinatus.
An anterior entry portal was made and shaver was introduced and debridement of the synovitis was performed. Chondroplasty of the humeral head, as well as the glenoid, was also performed. The scope was entered from the anterior portal and findings were re-confirmed and debridement was completed.
The scope was entered in the subacromial space. The tear was found in the supra and infraspinatus region. Debridement was done and the bursa was removed. There was an acromial spur anteriorly. The spur was removed by the use of electrocautery followed by burr.
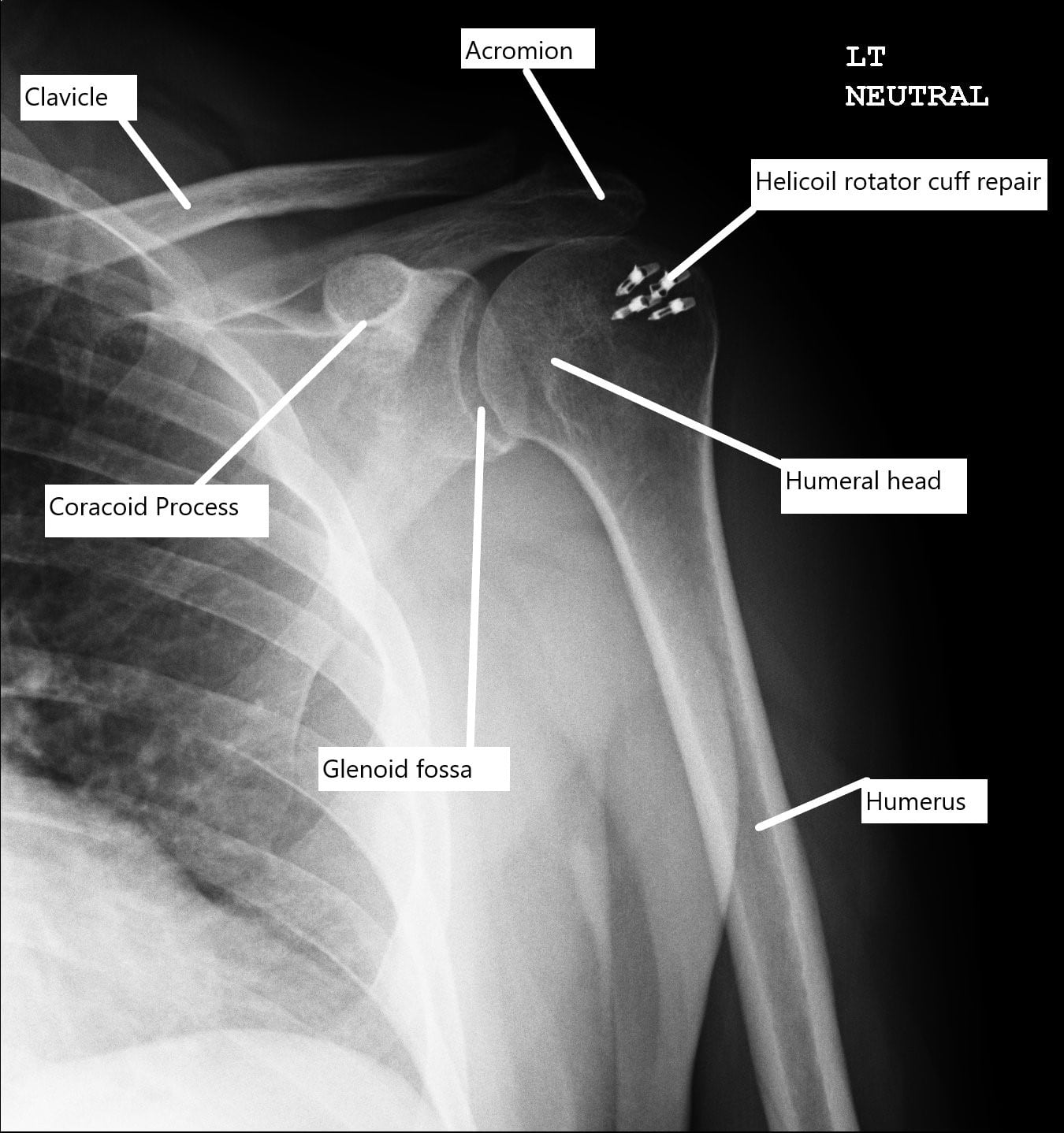
Postoperative X-ray of the shoulder with rotator cuff repair.
Acromioplasty was performed by removing the anterolateral acromial spur and as well as the inferior surface of anterior 2/3rd of the acromion. A decision was made to repair the rotator cuff. An accessory lateral portal was made. The footprint for the rotator cuff was debrided using a burr exposing the subcortical bone.
Then, a 4.5 mm Helicoil (S&N) with four tails was used and inserted into the humeral head following drilling and tapping. All the four tails were passed through the rotator cuff sequentially from the anterior to the posterior edge. The tails were tied over each over on to itself using a sliding knot.
The rotator cuff was well opposed. Final pictures were taken and saved. The shoulder was irrigated and drained.
Incisions were closed using #3-0 nylon. The dressing was performed using 4 x 4, ABD, tape. A shoulder immobilizer was applied after the surgery. The patient was extubated and moved to recovery in a stable condition.
Disclaimer – Patient’s name, age, sex, dates, events have been changed or modified to protect patient privacy.

Dr. Suhirad Khokhar
My name is Dr. Suhirad Khokhar, and am an orthopaedic surgeon. I completed my MBBS (Bachelor of Medicine & Bachelor of Surgery) at Govt. Medical College, Patiala, India.
I specialize in musculoskeletal disorders and their management, and have personally approved of and written this content.
My profile page has all of my educational information, work experience, and all the pages on this site that I've contributed to.
