Case Study: Lateral Meniscectomy in a 28 year-old male
An operation called a meniscectomy is performed to repair a meniscus that has been injured. A cartilage component called a meniscus aid in the appropriate function of your knee. The lateral meniscus is located on the outside of each knee and has two of them.
Meniscus tears can cause persistent knee discomfort, a sense that your knee is giving way, and limitations on how you can move your knee. Osteoarthritis in the damaged knee may be more prone to occur.
A 28 year-old male was in our office with complaints of pain in his neck, back, right leg and right arm. He remembers the injury to his neck, back, right leg and right arm due to a motor vehicle accident. The pain is moderate to severe in intensity. But he described the pain as sharp and aching.
The pain is associated with numbness, tingling, and radiating pain in the right upper and lower extremity (non-dermatomal). Walking, standing, lifting, exercising, using the stairs, and sitting make the symptoms worse. Pain medication makes the symptoms better. He has had a simulator place in his lower back for years. He is allergic to antibiotics, penicillin, sulfa and dicyclomine.
Upon examination of the right knee, the patient is tender to palpation along the medial and lateral facets of the patella. They have crepitus of the patellofemoral joint with range of motion and discomfort with patella grind testing. The patient has no discomfort with McMurray’s maneuvers, and the knee is stable but has a limited range of motion.
After a week he visited and told me that he had a fall 5 days back when his right knee gave way, following which he injured his right knee. He got X-rays in right knee. He is limping due to pain. Activities make the pain worse. He has been icing and elevating, which helps. His movement is restricted.
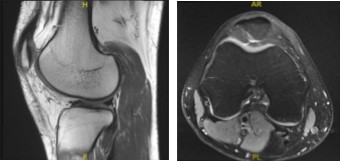
MRI-3T Right knee Non-contrast
On his MRI results it showed trace joint effusion and minimal patellar chondromalacia. Unremarkable MRI examination of the right knee.
We discussed the treatment options for the patient’s diagnosis, which included living with the extremity as it is, organized exercises, medicines, injections and surgical options. We also discussed the nature and purpose of the treatment options along with the expected risks and benefits.
I educated the patient regarding the inherent and unavoidable risks which include, but are not limited to anesthesia, infection, damage to nerves and blood vessels, blood loss, blood clots, and even death were discussed at length.
We also talked about the possibility of not being able to return to prior activities or employment, the need for future surgery, and complex regional pain syndrome. The patient also understands the risks of re-tear or failure to heal.
We also discussed the surgical procedure as well as the realistic expectations regarding the risks, outcome and post operative protocol. Plan: Arthroscopic examination of the knee, PF chondroplasty and all indicated procedures.
The patient was taken to the operating room where he was placed on the well-padded operating table. General anesthesia was Induced. The right knee was prepped and draped aseptically in the usual fashion. The tourniquet was applied on the lower thigh. An Esmarch was applied including 2.50. Preoperative antibiotic was given.
We pulled the patient on tourniquet 2.53. Laterally a working portal was made and using a 2.58 incision. Examination of the patellofemoral joint showed arthritis and posterior surface of the patella as well as on the trochlea. Examination of the medial Joint space showed medial femoral condyle arthritis, grade 2 to grade 3. Patellofemoral finding was also grade 3.
The scope was moved to 3.26 and found to be intact. Lateral compartment was examined and found to have a tear of the lateral meniscus, medial margin. The medial entry portal was made with direct access to the lateral condyle using a spinal needle. The lateral meniscus was trimmed using a shaver.
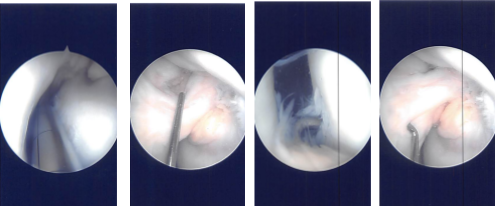
Intraoperative Arthroscopy Images
Chondroplasty of patellofemoral joint, medial femoral condyle was also performed using shaver. The knee was thoroughly irrigated. The closure was done by 4-0 and 3-0 nylon. Injection of 80 mg of Depo-Medrol and 19 mL of Xylocaine was performed. Dressing was done using 4 x 4, ABD, Webril, and ACE wrap. The patient extubated and moved to the recovery area in stable condition.
The patient was seen for post operative check up. We have decided to do formal physical therapy as well as a home exercise program for rehabilitation of the knee. We will continue to utilize early mobilization and mechanical prophylaxis to reduce the chances of a deep vein thrombosis.
The patient regularly followed an office visit every 3-4 weeks. Patient did well after the surgery and continued physical therapy. Patient checked in for a follow up visit after a month and saw significant improvement on his knee.
Disclaimer – Patient’s name, age, sex, dates, events have been changed or modified to protect patient privacy.

Dr. Vedant Vaksha
I am Vedant Vaksha, Fellowship trained Spine, Sports and Arthroscopic Surgeon at Complete Orthopedics. I take care of patients with ailments of the neck, back, shoulder, knee, elbow and ankle. I personally approve this content and have written most of it myself.
Please take a look at my profile page and don't hesitate to come in and talk.
