Case Study: ACL, Arthroscopic Assisted Reconstruction
with Autograft in a 59 year-old female
Surgeons use arthroscopic surgery, which is less intrusive and hastens patient recovery, to repair the ACL. The torn ligament is restored during an ACL reconstruction with a tissue graft from either a donor (allograft) or your own body (autograft).
A 59 year-old female patient who was going down the stairs when she missed a step complains of pain in her left knee. She buckled and experienced instability in her left knee.
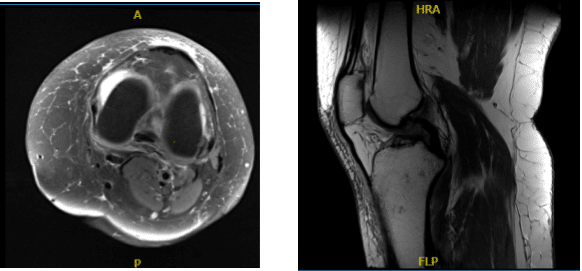
We performed an MRI, which revealed a high-grade partial ACL injury. Take into account that the patient was young, sick, and we talked about our alternatives. The knee also had very little arthritis. Treatment alternatives were explored, including well-known surgical management.
The patient chose a well-known surgical procedure. Infection, bleeding, damage to nearby nerves and blood vessels, surgical failure, the need for repeat surgery, arthritis, the need for knee replacement in the future, the need for knee rehabilitation, systemic complications including blood clots, cardiac outcome, and neurological complications including death were some of the risks and benefits we discussed. The client was aware and gave informed consent.
MRI-3T Left Knee non-contrast
The patient was brought into the operating room and laid out on a sturdy operating table. Anesthesia was induced throughout. After aseptically accessing the left lower extremity, a thigh-high tourniquet was put on the left side and examined. A timeout was ordered.
1 g of tranexamic acid and preoperative antibiotics were administered. After the procedure, another gram of tranexamic acid was administered. An lateral entrance portal was created using a scalpel, and an arthroscopic examination of the patellofemoral compartment revealed that the patella’s cartilage was still intact.
The trochlea has arthritis in grade 1. When the medial tibiofemoral compartment was examined, the meniscus and cartilage were both in good condition. Additionally, the meniscus and cartilage examined in the lateral tibiofemoral compartment were in good condition.
Examination of the intercondylar notch showed high-grade partial tear of the ACL. Decision was made to do the reconstruction of the ACL with a quad tendon. Arthroscope was removed and incision was given over the distal thigh anteriorly from the superior pole of patella up and below.
Sharp dissection began onto the quadriceps tendon. Quadriceps tendon stripper of 10 mm was taken from Arthrex and tendon was cut for about 70 mm. Sharp dissection was done to respect the graft from the tendon initially.
A FiberTak was used to connect it to the femoral end of the tendon for the preparation of the graft. Now, the cigar cutter was used to dissect the tendon further and about a 65-mm tendon was cut.
On the back table, the tendon was prepped with FiberTak on the opposite side as well. To prevent fluid leakage caused by iatrogenic opening of the joint capsule during the procedure, the proximal wound was closed in the interim. Back into the knee, the arthroscope was introduced, and the ACL was debrided on both the femoral and tibial sides.
The femoral ACL jig was placed from the lateral portal following complete debridement. An external sleeve was placed, and a skin incision was made. To the bone, the sleeve was inserted. A femoral tunnel was created using the Flip Cutter. After flipping the cutter, a 30-mm tunnel was created overall in fashion.
The FiberLoop was used to tag the canal. In a similar manner, the medial portal was now used to insert the tibial jig, and a sleeve was used to designate the skin incision. The sleeve was placed onto the bone following the skin incision.
The tunnel was constructed once more using a FlipCutter. The gutter was flipped once the drill had been inserted, and a 25 mm tunnel was created. The tunnel appeared to be a little too short. FiberStick was once more used to label the tunnel.
To accommodate the graft, the medial entry site for the arthroscope P was widened. The same medial portal was used to feed the FiberStick loops through, along with loading and passing the femoral side of the quadriceps tendon to the femoral tunnel and retrieving and flipping a button. In order to allow the tendon to flow into the tunnel, the TightRope RT was gradually tightened.
Now the button was reversed and the quadriceps’ tibial end was similarly passed. The quadriceps side was effectively tightened. On the tibial side, which was taut when the sutures were under tension, there was some loosening.
There were 30 cycles of the. #4.75 SwiveLock was used to immerse the sutures into the tibia. It was possible to get a good strain on the ACL, and photos were taken and preserved. With the aid of chondral, a microfracture chondroplasty was carried out to release bone marrow and promote quick healing.
After two weeks the patient was seen in the office for her postoperative visit. Her pain is improving and she is using crutches and knee immobilizer. After discussing treatment options, we have decided to proceed with formal physical therapy as well as a home exercise program for rehabilitation of the knee.
We went over the arthroscopic pictures and removed the stitches during the visit. We will continue with ice and elevation of the knee to decrease swelling and pain. We will continue to utilize early mobilization and mechanical prophylaxis to reduce the chances of a deep vein thrombosis.
We will wean them off any narcotic medications and progress to anti-inflammatories and Tylenol as long as there are no contraindications to these medications. We also discussed the risk and benefits and common side effects of taking these medications. The patient will be back in three weeks’ time to evaluate their progress.
The patient was seen in the office after one month of her postoperative visit. Her pain is improving though she is using a cane and knee immobilizer. She is working with Advanced PT and improving in her ROM and strength. She is an assistant principal and plans to go back to work with restrictions.
We discussed treatment options including PT, MRI, Injection, surgery. We agreed to go with conservative management for now. PT to be continued, Ice/heat, Elevation and taking OTC anti-inflammatory meds. Follow up checkup every 4 weeks.
With regular visits and attending physical therapy and home exercises for the knee, the patient gets well and recovered.
Disclaimer – Patient’s name, age, sex, dates, events have been changed or modified to protect patient privacy.
I am Vedant Vaksha, Fellowship trained Spine, Sports and Arthroscopic Surgeon at Complete Orthopedics. I take care of patients with ailments of the neck, back, shoulder, knee, elbow and ankle. I personally approve this content and have written most of it myself.
Please take a look at my profile page and don't hesitate to come in and talk.