Case Study: Knee Arthroscopy: Medial and
Lateral Meniscal Repair in a 21 year-old female
On the inside of the knee joint is the medial meniscus. On the outside of the knee is the lateral meniscus. Size and severity of meniscus tears can vary significantly. A meniscus might be torn in half, have a C-shaped rip around its perimeter, or be left attached by a thread to the knee joint.
If the cartilage surfaces are still in reasonably excellent condition, radial or lateral meniscus root rips should be corrected. In order to repair this, scar tissue must be removed, the meniscus must be pulled back into the joint, and depending on the type of tear, it must either be sutured together or tacked to the bone.
The patient is a 21-year-old female whom I have seen several times in the office. She was in a car accident and developed pain on the inner side of her left knee as a result. She tried conservative treatment, which did not work. An MRI was performed, which revealed a left knee medial meniscus tear.
We examined treatment alternatives and decided on surgical intervention. We reviewed the dangers and benefits, as well as consequences such as infection, hemorrhage, nerve and vascular injury, surgery failure, the necessity for repeat surgery, and the development of arthritis, among others.
We talked about systemic concerns such as blood clots, cardiac, pulmonary, and neurological issues. The informed consent was understood and signed by the patient.
The patient was brought to the operation room and placed on a well-padded operating table. Anesthesia was administered. As is customary, the left lower extremity was prepped and draped aseptically. A timeout was provided. The tourniquet was raised.
An arthroscope was introduced through a lateral entrance hole. The spinal needle was used to create the medial entrance portal. The medial meniscus was examined and found to have a peripheral tear along the body of the meniscus.
There was no injury to the cartilage. The ACL was found to be intact when the intercondylar notch was examined. Fraying of the posterior horn of the lateral meniscus was discovered during an examination of the lateral tibiofemoral compartment.
The cartilage was not damaged. The patellofemoral compartment was found to have complete cartilage. It was chosen to repair the medial meniscus tear. The tear was prepped with a rasp and shaver, and a FasT-Fix and arthroscopy were introduced through the lateral portal and the medial portal, respectively.
A horizontal mattress suture was placed and then cut. Fixation was successful. Photographs were taken and preserved. The lateral meniscus posterior horn was also shaved, and photographs were taken and stored.
Chondroplasty picks were used, as well as four microfractures, to allow bone marrow venting. Fat globules, followed by blood, could be observed venting out of the holes to help the meniscus mend faster. The final photographs were shot and preserved. The knee had been completely irrigated and drained.
The 3- 0 nylon was used for the closure. The knee was then injected with 20 mL of 0.5% Marcaine. Dressing materials included 4×4, ABD, Webril, and Ace wrap. A knee immobilizer was worn. The patient was extubated and transferred to recovery in good condition.
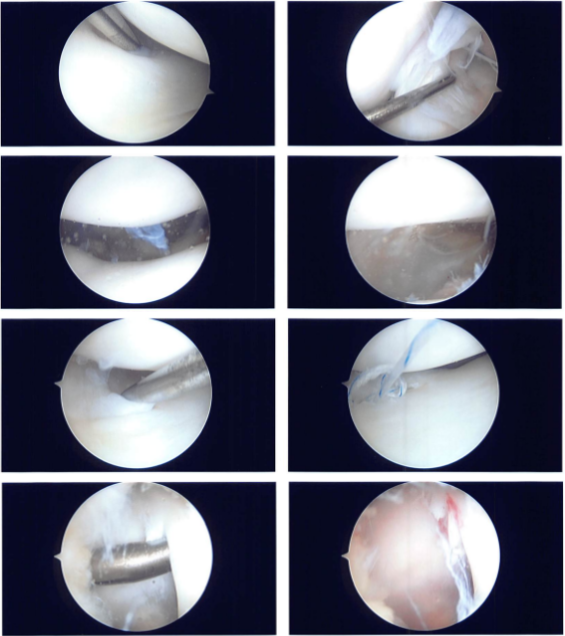
Intraoperative Images
The patient went to the office for her one-week post op visit. She denies fever or chills. She is using a knee immobilizer and occasionally ambulating without a brace. She has been complaining of numbness around the knee since the surgery.
We opted to proceed with official physical therapy as well as a home workout regimen for knee rehabilitation after examining treatment choices. During our current visit, we reviewed the arthroscopic images and removed the stitches. We will continue to use ice and elevate the knee to reduce swelling and pain.
To limit the risk of deep vein thrombosis, we will continue to use early mobilization and mechanical prophylaxis. We will gradually wean them off any narcotic medications and transition them to anti-inflammatories and Tylenol as long as there are no contraindications.
During the present appointment, we also addressed the risks, advantages, and common adverse effects of taking these medications. The doctor meets them again in three weeks to assess their improvement. They will contact us in the meantime if they have any questions or concerns before their follow-up appointment.
The patient seen by the doctor for her three weeks scheduled post operative visit. Just like before, she denies fever or chills. She is using a knee immobilizer. The numbness around the knee since the surgery is improving gradually. We discussed treatment options including PT, MRI, Injection, surgery and we agreed to go with conservative management for now.
After two months, the patient visits the office for her post op visit. She has no fever or chills, she is still using knee immobilizer. The numbness around the knee since the surgery is resolved and she has no knee pain or restriction of movement at present; she is working now with her PT.
She is presently working with PT and making good strides. The patient’s progress and development have been undeniable with continued physical treatment and regular attendance at his follow-up checkups.
Disclaimer – Patient’s name, age, sex, dates, events have been changed or modified to protect patient privacy.

Dr. Vedant Vaksha
I am Vedant Vaksha, Fellowship trained Spine, Sports and Arthroscopic Surgeon at Complete Orthopedics. I take care of patients with ailments of the neck, back, shoulder, knee, elbow and ankle. I personally approve this content and have written most of it myself.
Please take a look at my profile page and don't hesitate to come in and talk.
