Case Study: Knee Arthroscopy with Lateral Release
Chondroplasty and Osteophyte Excision
in a 31 year-old female
Lateral release surgery of the knee is an arthroscopic procedure that involves three tiny incisions in the knee. A lateral release is an arthroscopic operation used to help treat patella tracking issue caused by a tight lateral retinaculum. To allow the patella to track correctly, the lateral retinaculum is “released” or separated.
The patient is a 31 year-old female, who was seen in the office with complaints of right knee patellofemoral pain for many months. She has tried conservative management but has no relief.
X-rays were done, the distal femur, patella, proximal tibia and proximal fibula demonstrate intact cortical margins with no acute fracture. The medial, lateral and patellofemoral joint spaces are well-maintained. There is mild medial osteophyte formation. There is mild patellofemoral osteophyte formation.
There is no radiographic evidence of a joint effusion. There is no radiographic evidence of soft tissue swelling. The impression is there are mild osteoarthritic degenerative changes. There are no acute fractures.
Which showed lateral tilt of the patella towards the trochlea along with advanced patellofemoral arthritis with mild medial compartment arthritis. Also, the MRI was done to confirm the findings.
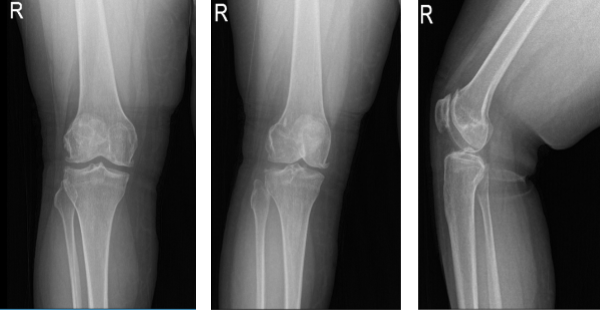
Right knee X-ray AP Lateral and Oblique 3 views
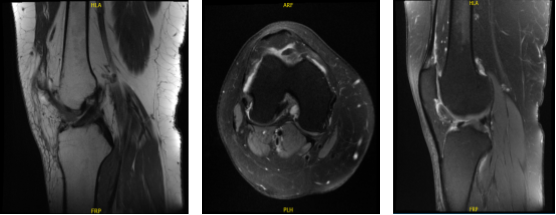
MRI-3T Right knee non-contrast
Treatment options were discussed with the patient including surgical and nonsurgical treatment. The patient opted for surgical management. We discussed lateral release along with chondroplasty. We also discussed that this may give her some temporary relief for a few months to years.
She may need knee replacement surgery done in the future. We discussed risks and benefits including infection, bleeding, injury to adjacent nerves and vessels, knee swelling, need for aspiration, non-relieving of the knee pain, need for rehabilitation, physical therapy, and need for knee replacement in the future amongst others.
The patient understood and signed an Informed consent.
The patient was taken to the operating room where general anesthesia was induced. Preop antibiotics were given. Tourniquet was applied in the right upper thigh. Esmarch was applied and tourniquet was elevated. Right lower extremity was prepped and draped aseptically in the usual fashion.
Time-out was called. Incision was driven over the central paravertebral region for entry of the arthroscope. Arthroscope was entered and an examination of the knee was done. A medial entry portal was made with the use of a spinal needle.
Examination showed intact medial and lateral meniscus as well as intact medial and lateral compartment. There were grade 3 to grade 4 osteoarthritic changes in the trochlea as well as patella. The lateral surface of the patella was denuded cartilage.
There was an osteophyte over the medial femoral condyle which was excised with the use of shaver and burr. Shaver was used to perform chondroplasty. The Coblation wand was also used to perform the chondroplasty. The patellar maltracking could be seen. Decision was taken for lateral release.
Arthroscope was entered through the medial portal and Coblation wand from the lateral portal. Lateral release of the capsule was performed from proximal to distal. All the bleeders were cauterized. Tourniquet was released at the end of the procedure. There was no active bleeding.
The border was also cut out and drained. There was no active bleeding. The knee was irrigated thoroughly and drained. Closure was done using # 3-0 nylon. Marcaine 9 cc mixed with 1 cc of 40 mg of Depo-Medrol was injected into the knee.
The patient’s dressing was done using 4x4s, ABD, Webril, and Ace wrap. The patient was extubated and moved to recovery in a stable condition.
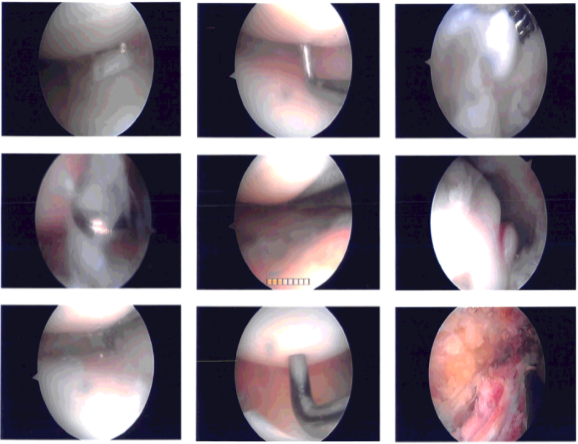
Intraoperative photo
After one week, the patient was seen in the office for her post operative visits, the patient is doing well, she denies fever, chills, her pain is well controlled and she is ambulating WBAT without aid.
After discussing treatment options, we have decided to proceed with formal physical therapy as well as a home exercise program for rehabilitation of the knee. We went over the arthroscopic pictures and removed the stitches during today’s visit.
We will continue with ice and elevation of the knee to decrease swelling and pain. We will continue to utilize early mobilization and mechanical prophylaxis to reduce the chances of a deep vein thrombosis. We will wean them off any narcotic medications and progress to anti-inflammatories and Tylenol as long as there are no contraindications to these medications.
We also discussed the risk and benefits and common side effects of taking these medications at today’s visit. I will see them back in three weeks’ time to evaluate their progress.
After one month the patient was seen for her follow up checkup, we agreed to go with conservative management for now. She is working with PT and has been improving but started having pain after PT last session due to weights and she is doing limited home PT, like a Stationary bike that can be used to help recover.
With the continued follow up checkup the patient showed progress from time to time she visits the office. She gets well after the surgery and with the help of continued physical therapy.
Disclaimer – Patient’s name, age, sex, dates, events have been changed or modified to protect patient privacy.

Dr. Vedant Vaksha
I am Vedant Vaksha, Fellowship trained Spine, Sports and Arthroscopic Surgeon at Complete Orthopedics. I take care of patients with ailments of the neck, back, shoulder, knee, elbow and ankle. I personally approve this content and have written most of it myself.
Please take a look at my profile page and don't hesitate to come in and talk.
