Case Study: Right Shoulder Extensive Debridement
in a 40 year-old patient
Extensive Debridement Shoulder Surgery, the joint enlarges as a result, providing the surgeon with additional room to assess the injury. The surgeon fixes the injury by using specialized equipment. Loose or diseased cartilage is removed during a procedure known as debridement. Bone spurs may be removed if they are there.
Any typical movement, such as raising your shoulder above your head, is impossible. Your shoulder has the impression of being out of its socket. You can tell something is wrong with your shoulder joint.
A 40 year-old patient was in our office with complaints regarding left hip, right shoulder, lower back and neck pain due to a car accident. He had no pain before the accident. He has been doing PT with no relief.
He presented results for the right shoulder’s x-ray that showed acromioclavicular joint arthropathy. For his left hip, x-ray have shown mild acetabular over coverage. For cervical spine, mild reduction in disc space.
He also presented MRI results for his left hi which have shown tear of the posterior superior labrum at the 10 to 11 o’clock position. Morel Lavalee lesion in the posterior subcutaneous tissues superficial to the tensor fascia lata.
Recommend orthopedic consultation. Cartilage loss and cystic change in the posterior superior acetabulum. Acetabular over coverage. Left greater trochanteric bursitis.
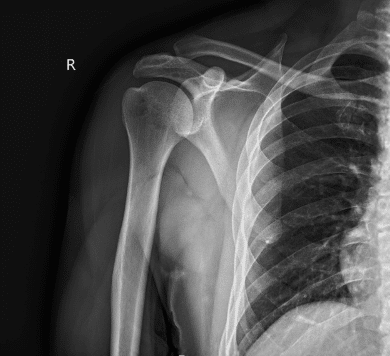
X-ray right shoulder minimum 2 views
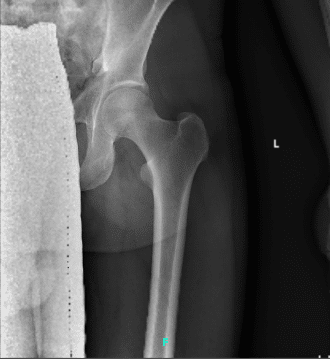
X-ray left hip 2-3 views
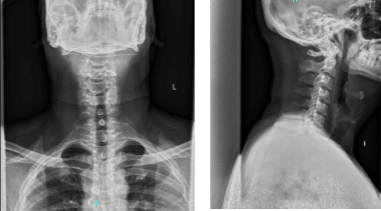
X-ray cervical spine 2 or 3 views
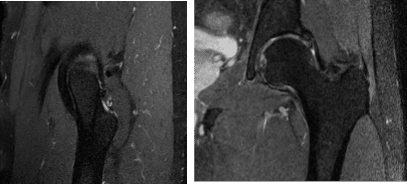
MRI Left Hip non-contrast
I discussed the treatment options for the patient’s diagnosis, which included living with the extremity as it is, organized exercises, medicines, injections and surgical options.
I also discussed the nature and purpose of the treatment options along with the expected risks and benefits.
I educated the patient regarding the inherent and unavoidable risks which include, but are not limited to infection, stiffness, damage to nerves and blood vessels, blood loss possibly requiring transfusion, blood clots, persistent or worsening pain, loosening or failure of implants, instability, tingling or numbness, anesthesia and systemic complications including cardiac, pulmonary, neurological complications and even death were discussed at length.
I also talked about the possibility of not being able to return to prior activities or employment, the need for future surgery, and complex regional pain syndrome. The patient also understands there is a long rehabilitative process that typically follows the surgical procedure.
I talked about the possibility of not being able to alleviate all the discomfort. Also, I explained there is no guarantee all the function and strength will return. I discussed the type of implants that may be utilized during this surgery.
The patient expressed understanding of these risks and has elected to proceed with surgery. I discussed the patient’s medications and allergies and the possible need for medical and other clearances if needed. I have discussed the surgical procedure as well as the realistic expectations regarding the risks, outcome and post operative protocol.
The patient was taken to the operating room where he was placed on a well-padded operating table. A supraclavicular block was given. General anesthesia was induced. The patient was put in the left lateral with the right shoulder up. Position was with the beanbag.
All the bony prominences were well padded. Axillary roll was inserted. The right shoulder was prepped and draped aseptically in the usual fashion. Preop antibiotic was given. Entry portal was made in the soft spot posterior to the glenohumeral joint.
Arthroscope was inserted through the entry portal. Anterior superoanterior entry portal was made with the use of a spinal needle and knife. A cannula was inserted through the anterosuperior portal. Examination of the glenohumeral joint showed partial tearing of the superior fibers of the subscapularis tendon.
There was glenoid labral fraying with no frank tear of the glenoid labrum. Debridement was done with the use of a shaver. Examination of the rest of the glenohumeral joint was intact. The arthroscope was inserted into the subscapularis space.
Shaver was inserted through the anterosuperior portal. Subacromial decompression was done with the use of a shaver. Examination of the rotator cuff of supraspinatus and infraspinatus showed intact tendons. There was a type 2 acromial spur.
Coblation wand followed by bur was used to perform the acromioplasty and remove the acromial spur. There was AC arthritis and capsular hypertrophy which was debrided with the use of Coblation wand followed by bur. Distal clavicle excision by removal of clavicle was performed.
The shoulder was thoroughly irrigated and drained. Closure was done with the use of #3-0 nylon. Dressing was done with the use of Xeroform, 4 x 4, ABD, and tape. The patient was put in a shoulder immobilizer, turned supine, extubated and moved to recovery in a stable condition.
The patient was seen for post operative check up. We have decided to do formal physical therapy as well as a home exercise program for rehabilitation of the shoulder.
Patients regularly followed an office visit every 3-4 weeks. Patient did well after the surgery and continued physical therapy. Patient checked in for a follow up visit after a month and saw significant improvement on his shoulder.
Disclaimer – Patient’s name, age, sex, dates, events have been changed or modified to protect patient privacy.

Dr. Vedant Vaksha
I am Vedant Vaksha, Fellowship trained Spine, Sports and Arthroscopic Surgeon at Complete Orthopedics. I take care of patients with ailments of the neck, back, shoulder, knee, elbow and ankle. I personally approve this content and have written most of it myself.
Please take a look at my profile page and don't hesitate to come in and talk.
