Case Study: Knee Arthroscopic Meniscectomy, Microfracture
Chondroplasty and Arthroscopic Assisted Tibial Plateau
Fixation with Calcium Phosphate Cement (Subchondroplasty)
Microfracture (Meniscus Repair, Knee Scope), Meniscectomy Knee arthroscopy is the process of using an arthroscope to look for general damage to the knee’s tissues and to heal specific ailments.
With good success, bone deficiencies in unstable tibial plateau fractures were filled with an injectable mineral bone cement that had a high initial mechanical strength. This information offers fresh viewpoints on how to treat tibial plateau fractures.
A 46-year-old patient presents with both shoulder, bilateral knees and back and neck pain with radiation into the right hand due to MVA. She is in status post left shoulder Arthroscopic Surgery performed a few months ago.
The surgery included rotator cuff repair, acromioplasty, subacromial decompression, distal clavicle excision and limited debridement. She denies fever, chills, her right shoulder and right knee were also hurting before this present accident that happened before.
She got a cortisone inj in right knee which had helped her. Now both her shoulders, both feet, both hips and both knees are hurting at present.
She is planned for arthroscopic assisted medial tibial plateau subchondroplasty. She has not been able to get an epidural injection recently due to fluid in back as per pain physician.
She got a cortisone injection in the neck which helped for 3 days. She is going to see a neurosurgeon. She is scheduled for a right knee subchondroplasty procedure.
After discussing the options for treatment and the risks of injection, the patient wished to proceed with the injection to reduce pain and swelling. After a sterile prep, 7cc of 1% Lidocaine and 80mg of depo-medrol were injected into the right shoulder subacromial space and left knee joint.
The patient tolerated the procedure well and there were no complications. Post injection pain, blood sugar elevation, skin discoloration, fatty atrophy and the signs of infection were discussed in detail. The patient was instructed to contact us if there were any questions or concerns prior to their follow up appointment.
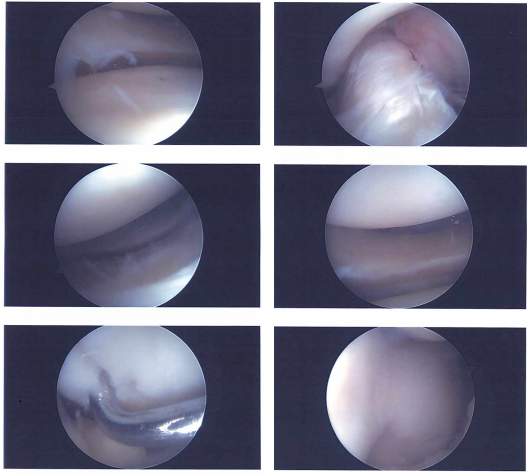
Image documentation
After two weeks the patient was seen in the office for her postoperative visit, she has no fever and chills. She got a cortisone injection in right shoulder and left knee which has helped.
After discussing treatment options, we have decided to proceed with formal physical therapy as well as a home exercise program for rehabilitation of the knee. We removed the stitches during the visit. We will continue with ice and elevation of the knee to decrease swelling and pain.
We will continue to utilize early mobilization and mechanical prophylaxis to reduce the chances of a deep vein thrombosis. We will wean them off any narcotic medications and progress to anti-inflammatories and Tylenol as long as there are no contraindications to these medications.
We also discussed the risk and benefits and common side effects of taking these medications. The patient will be back in three weeks’ time to evaluate their progress. We also agreed to go with conservative management for now, PT to continue and WBAT.
After three weeks the patient was seen in the office for her postoperative visit. The suture was removed with sterile forceps. After discussing the options for treatment and the risks of injection, the patient wished to proceed with the injection to reduce pain and swelling.
After a sterile prep, 1cc of 1% Lidocaine and 20mg of depo-medrol were injected into the left shoulder AC joint. The patient tolerated the procedure well and there were no complications. Post injection pain, blood sugar elevation, skin discoloration, fatty atrophy and the signs of infection were discussed in detail.
Status post right knee arthroscopic meniscectomy, microfracture chondroplasty and arthroscopic assisted tibial plateau fixation with Calcium phosphate cement (subchondroplasty) surgery performed. She is also status post left shoulder Arthroscopic Surgery performed.
The surgery included Rotator cuff repair, Acromioplasty, Subacromial decompression, Distal clavicle excision and limited debridement. She is planned for Right Shoulder Rotator cuff repair, Acromioplasty and distal clavicle excision.
We discussed at length to continue seeing a Neurologist for tremors and speech issues, Psychologist and psychiatrist for depression and anxiety, Pain physician for back and neck pain, primary care doctor for pedal edema. Will get an MRI for the chest for the nape of neck swelling in the supraclavicular region of both sides.
MRI were viewed and discussed; Thyroid: Unremarkable, without lesion, mildly limited assessment due to signal dropout over the neck region. Lungs: No focal lesion or diffuse lung pathology.
No pleural effusion. Mediastinum: No mediastinal or hilar adenopathy. Unremarkable cardiovascular structures. No pericardial effusion. No aortic aneurysm or coarctation. Patent arch great arteries.
Thoracic spine and chest wall: Mild dextrocurvature of the thoracic spine, otherwise unremarkable. Upper abdomen: No abnormality in the visualized portion of the upper abdominal organs.
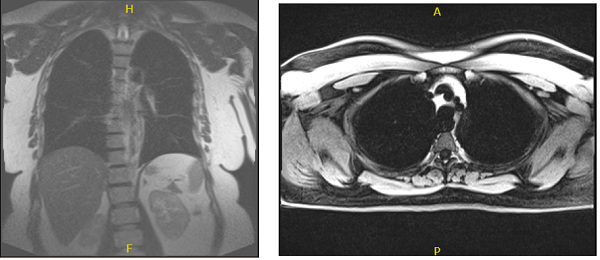
MRI chest without and with contrast
The patient was seen multiple times in the office for treatments and medications for her conditions to get well.
Disclaimer – Patient’s name, age, sex, dates, events have been changed or modified to protect patient privacy.

Dr. Vedant Vaksha
I am Vedant Vaksha, Fellowship trained Spine, Sports and Arthroscopic Surgeon at Complete Orthopedics. I take care of patients with ailments of the neck, back, shoulder, knee, elbow and ankle. I personally approve this content and have written most of it myself.
Please take a look at my profile page and don't hesitate to come in and talk.
