Case Study: Medial Meniscus Repair
performed to 45-year old female
The meniscus, once thought to be a non-function embryonic remnant, are now recognized to be critical for the normal function and long-term health of the knee joint. The meniscus help to stabilize the femorotibial articulation, spread axial load, absorb shock, and lubricate and nourish the knee joint.
Meniscus tears usually take place when an athlete twists or turns their upper leg while their foot is planted and their knee is bent. A meniscus tear occurs when an athlete twists or turns their upper limb while their foot is grounded and their knee is bent.
A torn meniscus can happen as a consequence of a car accident. In this instance, we will look at a medical meniscus repair that occurred for a female patient who was involved in a motor accident.
The patient is a 45-year-old female who has been complaining of right knee discomfort for over three weeks. The patient recalls being injured in a motor vehicle a year ago. The agony is excruciatingly painful. The discomfort is described as sharp by the patient. The pain is constant and interferes with slumber.
The condition is characterized by swelling, locking, weakness, and the inability to extend the knee. She walks with the assistance of an underarm crutch. There is no bruising, instability or giving way, crepitus, tingling, numbness, radiating pain, weakening, gait or bowel or bladder abnormality, or trouble with hand function.
The problem has grown worse since its inception. Standing, twisting, bending, squatting, kneeling, and descending steps aggravate the symptoms. Rest and elevation alleviate discomfort.
The patient’s right knee is tender to palpation along the medial joint line and has an effusion, according to an evaluation. On palpation along the medial and lateral PF joint lines, the patient also has PF crepitus and soreness. The patellar grinding test results are good. McMurray’s maneuvers cause pain in the patient, but the knee is stable.
Due to the effusion, they lack complete flexion but have full extension. They have 5/5 power and are distally neurovascularly intact. There is no erythema, heat, or cutaneous lesions. The patient’s contralateral extremity is nontender to palpation and has a good range of motion, stability, and strength.
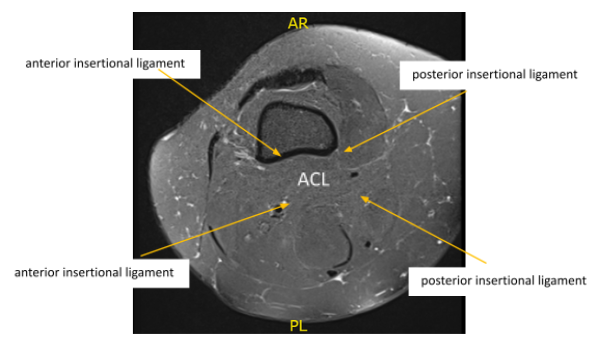
MRI reviewed. There is mild mucinous transformation of the ACL. is a longitudinal tear the posterior horn of the medial meniscus extending into the posterior root attachment site. See series 5 images 19-21. A small joint effusion is noted and mild patellar cartilage wear.

X-ray result showed Mild osteoarthrosis in the medial and anterior compartment of the knee.
We reviewed the patient’s treatment options, which included living with the extremity as is, organized exercises, medications, injections, and surgical options. We also talked about the nature and purpose of the treatment choices, as well as the potential risks and benefits.
The patient has expressed a desire to continue with surgery, which I believe is a viable option. I informed the patient about the inherent and unavoidable dangers, which included, but were not limited to: anesthesia, infection, nerve and blood vessel damage, blood loss, blood clots, and even mortality.
We also discussed the chance of being unable to resume previous activities or employment, the need for future surgery, and complex regional pain syndrome. The patient is also aware that a lengthy rehabilitative process usually follows the surgical treatment. We discussed the prospect of not being able to relieve all of the discomfort.
I also stated that there is no assurance that all function and strength will be restored. The patient is also aware of the dangers of re-tear or inability to heal. The patient is aware that implants may be used during this procedure. The patient acknowledged these risks and decided to continue with surgery.
General anesthetic was administered. Over the right lower limb, a tourniquet was applied. Aseptically, the right lower limb was prepped and draped and Esmarch applied too. The knee joint was inspected and a lateral entry portal was established. A medial meniscus peripheral rupture was discovered.
A grade 1 to grade 2 median condylar osteochondral lesion of the femur was also found. The ACL had some fraying and degeneration. the healing of the medial meniscus. Sutures from Fast-Fix were used. The peripheral laceration from the posterior horn to the mid body was repaired with seven sutures.
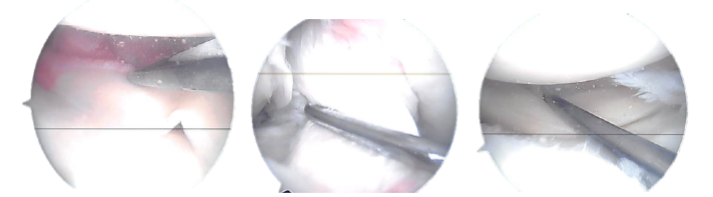
Actual Arthroscopic images taken during the operation
Final picture showing operative part dressed
Final arthroscopic pictures were taken. The knee was lavage with copious’ normal saline. The incision was cleaned with nylon 3-0 and dressed with Adaptic, 4 x 4, and BD, then with Webril and Ace bandage. The ligature was taken off. The patient was extubated and transferred to a stretcher to the postoperative care section.
After a week, the patient was seen with the knee brace extension suggested by the doctor. A small effusion is discovered on evaluation of the right knee. The wounds are mending well, with no signs of drainage, erythema, or warmth. Because of the discomfort, there is a restricted range of motion.
Distance strength is 5/5. There is no calf soreness and the Homan’s sign is negative. Distally, sensation is intact to light contact, and capillary refill is rapid.
We chose to continue with formal physical therapy as well as a home exercise program for knee rehabilitation after discussing treatment options.
We also removed stitches on the right knee. We will continue to use ice and elevate the leg to reduce swelling and pain. To minimize the risk of deep vein thrombosis, we will continue to use early mobilization and mechanical prophylaxis.
We will gradually wean them off any narcotic drugs and transition them to anti-inflammatories and Tylenol as long as there are no contraindications. Every 3-4 weeks, the patient returned to the office. The patient recovered well from the surgery and continued physical rehabilitation.
Disclaimer – Patient’s name, age, sex, dates, events have been changed or modified to protect patient privacy.

Dr. Vedant Vaksha
I am Vedant Vaksha, Fellowship trained Spine, Sports and Arthroscopic Surgeon at Complete Orthopedics. I take care of patients with ailments of the neck, back, shoulder, knee, elbow and ankle. I personally approve this content and have written most of it myself.
Please take a look at my profile page and don't hesitate to come in and talk.
