Case Study: Knee Arthroscopy: Medial Meniscectomy
Chondroplasty in a 65 year-old female
To diagnose and treat problems with the knee joint, a surgical procedure called knee arthroscopy may be used. To repair a damaged meniscus, a procedure known as a meniscectomy is carried out. Furthermore, the lateral meniscus acts as a shock absorber and helps the knee to stabilize.
It lubricates the joint and keeps it that way, normalizing joint motion to prevent knee hyperextension. In this collection of publications, we analyze medial meniscectomy chondroplasty in great detail.
Patient is in our office today complaining of left knee pain. She is 65 years of age and mentioned that she was seen by another surgeon in the past and she wants to have a second opinion on her knee condition.
She presented her MRI today, based on the findings, it clearly showed the small interior surface flap tear of the posterior horn of the meniscus, with degeneration and inferomedial extrusion of the posterior horn-body segment associated with reactive bone marrow edema in the underlying medial tibial plateau and reactive medial pericapsular soft tissue edema.
Also, there is mild to moderate medial compartment osteoarthritis with chronic osteochondral lesion over the posterior aspect of the medial femoral condyle. Degeneration of the medial is present, and moderate sized joint effusion.
We discussed the treatment options for the patient’s diagnosis, which included: living with the extremity as it is, organized exercises, medicines, injections and surgical options. We also discussed the nature and purpose of the treatment options along with the expected risks and benefits.
The patient has expressed a desire to proceed with surgery, and I think that is a reasonable option. I educated the patient regarding the inherent and unavoidable risks which include, but are not limited to: anesthesia, infection, damage to nerves and blood vessels, blood loss, blood clots, and even death were discussed at length.
We also talked about the possibility of not being able to return to prior activities or employment, the need for future surgery, and complex regional pain syndrome. The patient also understands there is a long rehabilitative process that typically follows the surgical procedure.
We talked about the possibility of not being able to alleviate all of the discomfort. Also, I explained there is no guarantee all the function and strength will return. The patient also understands the risks of re-tear or failure to heal. The patient understands implants may be utilized during this surgery.
The patient expressed understanding of these risks and has elected to proceed with surgery. Ample time was given for questions, of which many were addressed. We have discussed the surgical procedure as well as the realistic expectations regarding the risks, outcome and post operative protocol. Patient signed informed consent.
The patient was taken to the operating room where general anesthesia was induced. Left lower extremity was prepped and draped aseptically in the usual fashion. Tourniquet was applied. Esmarch was also applied.
Time-out was called. Preoperative antibiotic was given. A lateral incision was given for the entry portal. Scope was entered. Patellofemoral compartment showed grade 1 to grade 2 osteoarthritic changes.
A medical entry portal was made using a spinal needle. Examination of the medial compartment showed a complex tear of the posterior horn of the medial meniscus. The tear was debrided. Medial meniscus was debrided with the use of straight biter, upbiter, and shaver.
Examination of the intercondylar notch showed intact ACL with degeneration. Examination of the lateral compartment showed medial frayed margins of the lateral meniscus which was debrided with the use of upbiter as well as the shaver.
The debridement of the patellofemoral joint was done and chondroplasty was performed with the use of the thermal wand and shaver. Suprapatellar plica was permanent which was removed with the use of a thermal wand.
The scope was entered from the medial portal and instruments were entered from the lateral portal to complete the medial meniscectomy.
Final pictures were taken and saved. The knee was thoroughly irrigated. The knee was drained. Closure was done with use of the # 3-0 nylon. A 9 cc of Naropin 0.5% mixed with 40 mg of Depo-Medrol was injected in the knee.
Dressing was done with the use of Xeroform, 4 x 8, Webril, and Ace wrap. The patient was extubated and moved to recovery in a stable condition.
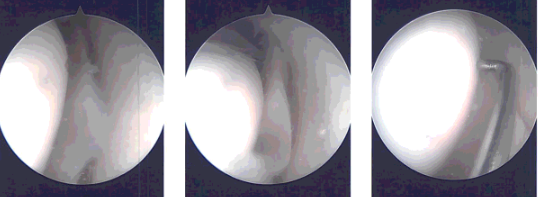
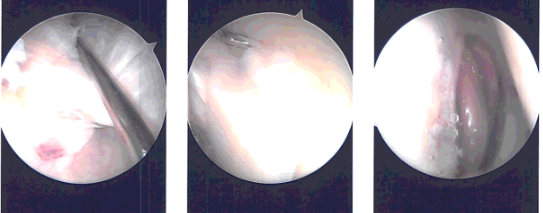
Intraoperative images
The patient was examined for a check-up following surgery. In order to rehab the knee, we have chosen to combine conventional physical therapy with a home exercise program. Every three to four weeks, the patient would attend the office as usual.
After the operation, the patient recovered well and kept up with physical therapy. After a month, the patient returned for a follow-up visit and his knee had much improved.
Disclaimer – Patient’s name, age, sex, dates, events have been changed or modified to protect patient privacy.

Dr. Vedant Vaksha
I am Vedant Vaksha, Fellowship trained Spine, Sports and Arthroscopic Surgeon at Complete Orthopedics. I take care of patients with ailments of the neck, back, shoulder, knee, elbow and ankle. I personally approve this content and have written most of it myself.
Please take a look at my profile page and don't hesitate to come in and talk.
