Case Study: Knee Arthroscopy: Medial Meniscal Repair
with the use of Semitendinosus Allograft and
Medial Femoral Condyle in a 30 year-old male
A fresh meniscus (taken from a cadaver) is implanted into a patient’s knee joint during a meniscus transplant. Technically, this process is referred to as a meniscal allograft transplant.
A simple definition of the term “allograft” is “the transplantation of tissue from one person (a donor) to another.” Within the knee joint, between the femoral condyles and the tibial plateau, are the medial and lateral menisci.
The 30-year-old patient male presents with left knee pain after a fall down the stairs one month ago. The patient reports he experienced immediate pain and swelling in the left knee. He states it felt that his kneecap may have popped out of place.
He did not seek any immediate medical treatment. He had a knee immobilizer and crutches at home which he applied to the knee. He has been using the crutches for assistance in ambulation.
He reports mild improvement in his symptoms but he continues to have severe pain and swelling in the knee. He denies numbness and paresthesia. No other complaints currently. He was seen by an ortho surg and MRI was done and he was advised surgery.
On a physical exam, the patient is awake, alert, and oriented, in no acute distress. Patient displays generalized ligamentous laxity. On examination of the left knee, there is a very large effusion present with no associated erythema or warmth. There are no open wounds or abrasions.
He has significant pain with palpation in the region of the MPFL and mild pain with palpation diffusely throughout the knee. He has pain and apprehension with patellar mobility. He is able to achieve range of motion from 0-60° with pain on attempts of any flexion beyond this point.
He appears to have stability to Lachman’s testing and to valgus and varus stress testing. He is unable to actively straight leg raises at this time secondary to pain and swelling.
There does not appear to be any palpable gap about the quadriceps tendon insertion and no pain in this region. Calf and thigh are soft and nontender and he is grossly neurovascularly intact distally with brisk capillary refill.
X-rays & MRI were reviewed and discussed by the doctor; Radiology Report: X-rays were performed in the office today of the left knee, 3 views, AP, lateral and sunrise views, reveals no evidence of acute fracture, dislocation or other osseous or articular abnormalities.
Impression: 30-year-old male with left knee likely status post patellar dislocation, evaluate MPFL and patella for occult fracture/loose bodies. We discussed treatment options and opted for surgical management.
We discussed risks including infection, bleeding, injury to adjacent nerves and vessels, numbness, need rehabilitation, need for possible failure, need for repeat surgery, need for secondary surgery, systemic complications like blood clots, cardiac, pulmonary, neurological complications including death. The patient understood and signed the informed consent.
The patient was taken to the operating room area and general anesthesia was induced. Left lower extremity was prepped and draped aseptically in the usual fashion. It was put in the C-clamp and the tourniquet was elevated. Preop antibiotic and tranexamic acid was given. A time-out was called.
A lateral entry portal was made. An arthroscope was inserted. There was hemarthrosis which was irrigated and drained. A ̧working medial entry portal was made with the use of spinal needle and shaver was inserted to complete the debridement.
Examination of the medial tibiofemoral compartment showed intact meniscus and intact cartilage. Examination of the intercondylar notch showed strain of the ACL. The ACL was intact, but loose.
Examination of the lateral tibiofemoral compartment showed intact cartilage and meniscus. Examination of the patellofemoral compartment showed a 1 cm x 1 cm osteochondral defect in the posterior surface of the inferomedial region of the patella.
The loose body was found in two pieces sitting in the trochlear notch. The loose body was excised with the use of the grasper through the medial portal. Chondroplasty of the patellar defect was then performed. Rest of the examination of the knee was normal. Knee was irrigated and drained.
Now the scope was removed and the knee was extended on the table. Further draping was performed. A triangle was used given the knee in a 30-degree position. A medial incision was given over the superior margin of the patella.
The incision was extended deep on to the medial margin of the superior half of the patella with the use of blade followed by Bovie. Two entry portals were made for the MPFL ligament. MPFL reconstruction: one at the midline and other at the 10 o’clock position.
After the holes were drilled, further reaming was performed for the insertion of the 4.75 SwiveLock. A semitendinosus allograft was prepared in the back table with tapered margins and #2-0 FiberLink used to whip stitch it.
The two ends of the tendon were inserted into the patella in either hole with the use of 4.75 mm SwiveLock. Now, the fluoro was brought in to mark the Schottle’s point and then medial incision was given over the fibula medial condyle.
After the dissection was taken deep to the medial femoral condyle, fluoro was again brought in and a template was used to mark the Schottle’s point. The Schottle’s point was marked just anterior proximal to the Intersection of the Blumensaat’s line with the posterior margin of the femur.
It was just distal to the adductor tubercle as well as the posterior condylar line of the femur. A Beath pin was used which was inserted from the medial condyle and driven proximally and anteriorly into the femur. Over reaming was performed for about 50 mm.
Plane was dissected in between the segment of the trochlea just outside of the capsular of the knee. The loop of the tendon was extracted along this plane into the medial incision. The loop was passed onto the Beath Pin with the use of FiberWire and the tendon was pulled into the tunnel.
Now, the #6-0 anchor was put over the digital wire onto the tunnel and the knee was put in 30-degree flexion, constant lateral pull on the patella was given to keep the tendon taut with the patella on to grade 1 movement of the patella laterally.
This was found to be tight in extension and loose in flexion. The Biocomposite screw was inserted completely into the tunnel in the desired position. The knee was reached from 0 degree to 110 degree and found to be stable.
The wounds were thoroughly irrigated and drained. Closure was done in layers using #0 Vicryl and # 2-0 Vicryl and nylon. Dressing was done with the use of the adaptic, 4 x 4s, ABD, and Webril; 20 cc of 0.5% Marcaine was injected into the knee before the closure. A knee immobilizer was applied in O degree flexion and locked. The patient was extubated and moved to recovery in a stable condition.
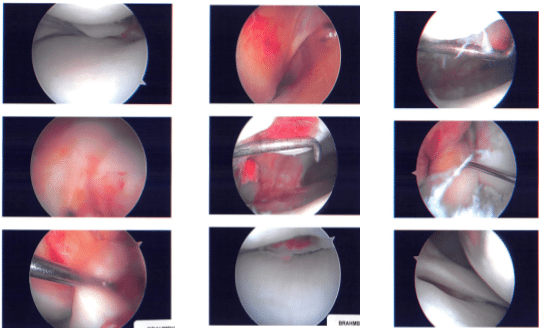
Intraoperative images
The patient is here today for his one-week post-operative examination, he denies fever, chill and he is ambulating with crutches and not putting much weight on the left LE. After discussing treatment options, we have decided to proceed with formal physical therapy as well as a home exercise program for rehabilitation of the knee.
We went over the arthroscopic pictures and removed the stitches during the visit. We will continue with ice and elevation of the knee to decrease swelling and pain. We will continue to utilize early mobilization and mechanical prophylaxis to reduce the chances of a deep vein thrombosis.
We will wean them off any narcotic medications and progress to anti-inflammatories and Tylenol as long as there are no contraindications to these medications. We also discussed the risk and benefits and common side effects of taking these medications. The patient will be back in three weeks’ time to evaluate the progress.
After a month the patient was seen in the office for his postoperative examination. He denies fever, chills. He is ambulating with crutches and putting full weight on the left LE and He is working with PT and improving.
The patient visits the office a couple of times, from the time to time of his visits he is gradually improving. Through regular visits and continued physical therapy, the patient healed and recovered.
Disclaimer – Patient’s name, age, sex, dates, events have been changed or modified to protect patient privacy

Dr. Vedant Vaksha
I am Vedant Vaksha, Fellowship trained Spine, Sports and Arthroscopic Surgeon at Complete Orthopedics. I take care of patients with ailments of the neck, back, shoulder, knee, elbow and ankle. I personally approve this content and have written most of it myself.
Please take a look at my profile page and don't hesitate to come in and talk.
