Case Study: Management of Ramp Lesion of the Medial
Meniscus with ACL Deficient Left Knee in a 30-year-old Female
The patient is in our office, with complaints of left knee pain for the past one year. The patient is a 30-year-old female who injured her knee while she was playing soccer a year ago. The pain got better over time but she reinjured again 6 months ago and has been having pain since then.
The pain is intermittent and does disturb sleep. The pain is associated with bruising. The pain is not associated with swelling, tingling, numbness, radiating pain, weakness, bowel or bladder abnormality, gait problem, giving way, or limping. The problem has been getting worse since it started.
Physical Therapy makes the symptoms better. The patient has not undergone any surgery in the past. The patient is currently taking Advil. The patient is a smoker.
On examination of the left knee, the patient is tender to palpation along the medial joint line and has an effusion. The patient has discomfort with McMurray’s maneuvers, and the knee is stable. They lack full flexion secondary to the effusion but have full extension. Bilateral lower extremities have 5/5 strength and are neurovascularly intact distally. There are no erythema, warmth, or skin lesions present.
On examination of the contralateral extremity, the patient is nontender to palpation and has an excellent range of motion, stability, and strength.
MRI examination of the left knee suggested a complex tear of the posterior horn of the medial meniscus. Small horizontal cleavage tear of the body of the lateral meniscus.Moderate joint effusion with synovitis.
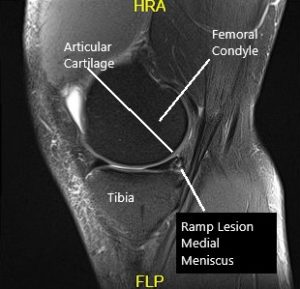
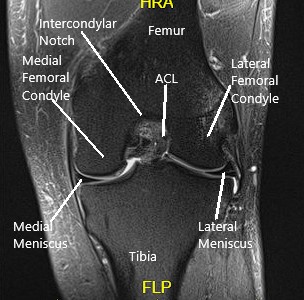
MRI of the knee in the sagittal and coronal section.
We discussed the treatment options for the patient’s diagnosis, which included: living with the extremity as it is, organized exercises, medicines, injections, and surgical options. We also discussed the nature and purpose of the treatment options along with the expected risks and benefits. The patient has expressed a desire to proceed with surgery.
The patient also understands there is a long rehabilitative process that typically follows the surgical procedure. The patient expressed an understanding of these risks and has elected to proceed with surgery. Smoking cessation advise was given to the patient.
We also discussed regarding possibility of ACL tear and repair Vs reconstruction of ACL. The patient opted for ACL rehabilitation for now. The patient understood the risks and benefits and signed informed consent.
PREOPERATIVE DIAGNOSES: Complex tear of the medial meniscus of the left knee and tear of the ACL of the left knee.
POSTOPERATIVE DIAGNOSES:
- Ramp lesion of the posterior body of the medial meniscus of the left knee.
- Horizontal tear and central tear of the posterior horn of the lateral meniscus.
- ACL deficient knee left side.
OPERATIONS:
- Meniscal repair of the medial meniscus of the left knee.
- Partial meniscectomy and meniscal repair of the horizontal tear of the lateral meniscus of the left knee.
- Microfracture of the trochlea.
DESCRIPTION OF PROCEDURE: A lateral entry portal was made. The scope was entered. The patellofemoral joint was found to be in good shape with no cartilage damage. The scope was taken to the medial gutter where there was a synovial flap. The medial compartment showed a ramp lesion of the posterior body of the medial meniscus. The root was intact. There was no cartilage loss.
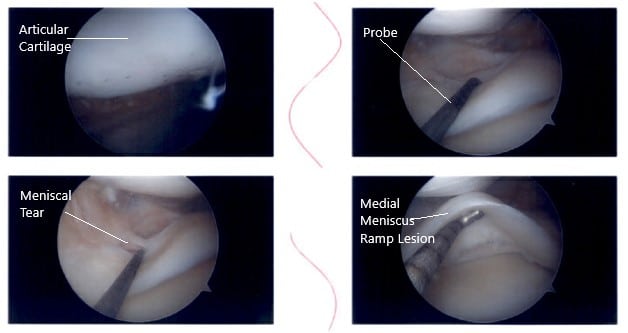
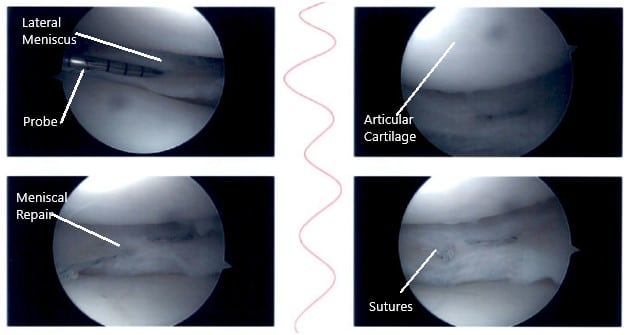
Intraoperative knee arthroscopic images.
The medial entry portal was made. The probe was inserted and the meniscus tear was again checked. It was involving the posterior body of the medial meniscus along with the capsule. The decision was made to repair the ramp lesion using an all-inside suture configuration.
Two curved and two reverse curved FasT-Fixes were used to complete the repair after the meniscus was abraded along with a capsule abrasion done with the shaver. The repair was found to be in a good position.

Intraoperative knee arthroscopic images.
Now the scope was moved to the internal trochlear area where ACL was deficient. Debridement was done. The scope was moved to the lateral compartment where we found medial edge fraying as well as a small bucket handle tear of the medial edge of the lateral meniscus. The medial edge was debrided.
Further examination showed a horizontal tear going up to the periphery of the lateral meniscus of the posterior body. The decision was made to repair this tear. Three FasT-Fixes were used for repair of the lateral meniscus, horizontal lesion. Before that, a posterolateral incision was given anterior to the fibula.
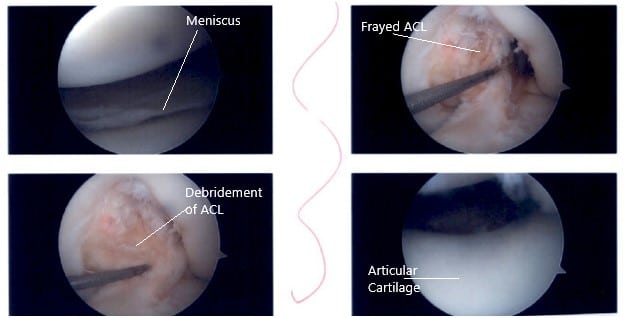
Intraoperative knee arthroscopic images.
With sharp and blunt dissection making a plane behind the LCL and between the knee capsule in the lateral head of gastrocnemius, a plane was made. Sims speculum was inserted to protect the posterior neurovascular bundles. After it was done, the scope was reentered and the repair of the left meniscus using FasT-Fixes was done in a satisfactory fashion. All the arthroscopic pictures were saved. Microfracture of the trochlear notch was performed using bundle fix.
Intraoperative knee arthroscopic images.
The tourniquet was released and bleeding bone could be seen from the microfracture site. Pictures were saved. The posterolateral wound incision was washed and closed. Hemostasis was achieved.
The closure was done in layers. The posterolateral incision was closed with Monocryl. The arthroscopic portals were closed using nylon. 20 cc of 05% Marcaine was injected in the knee. The dressing was applied. The knee was put in a knee mobilizer. The patient was extubated and moved to the postoperative care unit in good condition.
Disclaimer – Patient’s name, age, sex, dates, events have been changed or modified to protect patient privacy.

Dr. Suhirad Khokhar
My name is Dr. Suhirad Khokhar, and am an orthopaedic surgeon. I completed my MBBS (Bachelor of Medicine & Bachelor of Surgery) at Govt. Medical College, Patiala, India.
I specialize in musculoskeletal disorders and their management, and have personally approved of and written this content.
My profile page has all of my educational information, work experience, and all the pages on this site that I've contributed to.
