Case Study: Shoulder Arthroscopy with Biceps Tenodesis
in a 56 year-old male
A minimally invasive procedure called arthroscopic biceps tenodesis is used to fix and rejoin torn biceps tendons. Probably the most well-known muscle in the body is the biceps.
A sign of authority, it even has a flexed arm emoji to enhance its intimidating appearance. used to treat a shoulder’s biceps tendon rupture or partial tear. The Long Head of Biceps (LHB) tendon is reattached to the top of the humerus during this treatment, which relieves pain, discomfort, and gives the arm stability and strength.
The patient is a 56 year-old male who has been seen multiple times in the office for right shoulder pain. This pain started after the car accident. The surgery was planned, but could not be undergone earlier. The pain persisted and the patient came back to the office.
MRI was presented and discussed; Insertional tendinosis with a partial thickness tear of the anterior insertional footprint of the supraspinatus tendon. Tendinosis of the infraspinatus. Tendinosis with low-grade interstitial partial tear of the distal subscapularis. Teres minor is intact. No atrophy.
Intramuscular cyst at the myotendinous junction of the supraspinatus compatible with interstitial delamination fear. Hypertrophic changes of the AC joint with a lateral downsloping type II acromion and narrowing of the subacromial space. Findings likely act as a substrate for impingement.
Proximal biceps tenosynovitis. Diffuse tear of the superior, anterior, and posterior labrum. Glenohumeral joint osteoarthritis with spurring along the inferior aspect of the humeral head and glenoid and broad-based chondral loss. Small glenohumeral joint effusion.
Mild subacromial subdeltoid bursitis Fibrocystic changes present at the greater tuberosity. No acute fracture. No Hill-Sachs or Bankart lesions. Intact deltoid. Intact spinoglenoid and suprascapular notch. Thickening of the anterior band of the IGHL compatible with chronic inferior capsular sprain.
Impression: the Insertional tendinosis with a partial thickness tear of the anterior insertional footprint of the supraspinatus tendon. Tendinosis of the infraspinatus. Tendinosis with low-grade interstitial partial tear of the distal subscapularis.
The Intramuscular cyst at the myotendinous junction of the supraspinatus compatible with interstitial delamination tear. And the Hypertrophic changes of the AC joint with a lateral downsloping type II acromion and narrowing of the subacromial space. Findings likely act as a substrate for impingement.
Proximal biceps tenosynovitis. Diffuse tear of the superior, anterior, and posterior labrum. Glenohumeral joint osteoarthritis with spurring along the inferior aspect of the humeral head and glenoid and broad-based chondral loss.
Small glenohumeral joint effusion. Mild subacromial subdeltoid bursitis. Fibrocystic changes present at the greater tuberosity. Thickening of the anterior band of the IGHL compatible with chronic inferior capsular sprain.
We discussed treatment options and opted for surgical management. We discussed risks and benefits including infection, bleeding, injury to adjacent nerves and vessels, numbness, shoulder rehabilitation, shoulder receptors, failure and need for repeat surgery, systemic complications including blood clot, cardiac, pulmonary, neurological complication including death, the patient understood and signed and informed consent.
The patient was taken to the operating room where general anesthesia was induced. The patient was put in a left lateral position with the right shoulder up. Preop antibiotic and tranexamic acid was given. Timeout was called. The right upper extremity was put in traction of 10 pounds.
The arthroscope was made from the posterior soft spot. Biceps tendon, intra articular portion and the labrum had extensive fraying. Shaver was used for labral debridement. The rotator cuff was intact.
Debridement of subscapularis tendon as well as chondroplasty of the glenoid and humeral head was also performed. Arthroscope was inserted into the subacromial region and a shaver was inserted from the front and debridement with subacromial bursectomy was performed with a shaver. Acromial spurring was present, which was cleaned by the use of Coblation wand and #6.0 bur performing acromioplasty.
The AC joint also showed arthritic changes and so distal clavicular excision was done by excising about a centimeter of distal clavicle with the use of shaver from the posterior anterior portal. Examination of the rotator cuff was performed, which showed partial thickness rotator cuff tear.
It was of low grade and debridement was performed with the use of shaver. Considering the patient’s labile diabetes, it was decided not to use any implant to repair further. The final pictures were saved and the arthroscope was removed.
The shoulder was irrigated and drained. Plan for mini open tenodesis was performed and the patient’s arm was taken out of the traction and put in flexion and external rotation. Incision was given along the clear margin of the pectoralis major in the axilla along the anterior border of the axilla.
Deep fascia was cut in the line of incision. Subpectoral approach was used to reach the bicipital groove. The biceps tendon was delivered out of the wound. FiberLoop was used to put sutures from the musculotendinous junction and the excess of biceps tendon was removed.
The bicipital groove was cleaned with the use of Bovie and insertion point was marked with appropriate tension. Bicortical beat pin followed by a cortical hole with an 8 mm drill for the screw was made. The tendon sutures were passed onto the button and button inserted bicortically and flipped.
The suture ends were tightened and a needle was used to pass through the tendon and knotted. The biceps tendon was found to be in appropriate tension. a 7mm unicortical screw was further inserted to enhance the fixation.
The wound was thoroughly irrigated and drained. Closure was done in layers using #0 Vicryl, #2-0 Vicryl, and 3-0 monocryl; arthroscopic wounds were closed with #3-0 nylon. Dressing was done with use of Adaptic, 4×8, ABD, tape. The patient was put in a shoulder sling and moved to recovery in a stable condition.
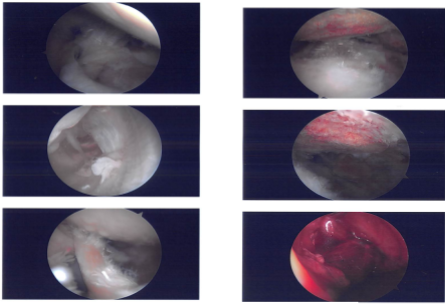
Intraoperative Images
After one week, the patient seen in the office for his post operative visits had no x-rays needed. The patient denies fever, chills, He is not wearing the shoulder sling and his pain has been improving.
After discussing treatment options, we have decided to proceed with formal physical therapy as well as a home exercise program for rehabilitation of the shoulder. We went over the arthroscopic pictures and removed the stitches during the visit.
We will continue with ice and elevation of the shoulder to decrease swelling and pain. We will wean them off any narcotic medications and progress to anti-inflammatories and Tylenol as long as there are no contraindications to these medications.
We also discussed the risk and benefits and common side effects of taking these medications. The patient will be back in three weeks’ time to evaluate the progress.
After a month the patient is seen in the office for his postoperative consultations, no x-rays needed, He does not have fever or chills. He is not wearing the shoulder sling; his pain has been improving and he is working now with his physical therapy.
The patient did well after the surgery, from the time to time of his visits he is gradually improving. Through regular visits and continued physical therapy, the patient healed and recovered.
Disclaimer – Patient’s name, age, sex, dates, events have been changed or modified to protect patient privacy

Dr. Vedant Vaksha
I am Vedant Vaksha, Fellowship trained Spine, Sports and Arthroscopic Surgeon at Complete Orthopedics. I take care of patients with ailments of the neck, back, shoulder, knee, elbow and ankle. I personally approve this content and have written most of it myself.
Please take a look at my profile page and don't hesitate to come in and talk.
