Case Study: Meniscal root repair in a 53-year-old female
Meniscal root rips are an increasingly common injury that, if left untreated, can result in significant functional restrictions, fast cartilage degeneration in the afflicted compartment, and a subsequent risk of complete knee replacement.
Meniscal extrusion frequently happens in conjunction with root tears, which impairs the transfer of circumferential hoop loads. This dramatically raises tibiofemoral contact pressure and modifies the kinematics and biomechanics of the knee.
Meniscus root repairs are done by isolating the root, stitching at least two sutures into the remaining meniscal connection, and then attempting to move the root back into a more anatomical location. The meniscus posterior horn may occasionally need to be freed from scar tissue to be relocated.
A 53-year-old patient was in our office, with complaints of left knee pain. The patient stated there was fluid in her knee. The pain is mild to moderate in intensity and described the pain as sharp. The pain is intermittent.
The pain is associated with swelling and limping, but the pain is not associated with bruising, tingling, numbness, radiating pain, weakness, bowel or bladder abnormality, gait problem, giving way, or hand function difficulty.
The problem has been getting worse since it started. But with the help of ice, and inflammatory medication makes the symptoms better. The patient has undergone surgery twice but did not want to state over the phone. Patient has no allergies and does not smoke.
Upon examination of the left knee, the patient is tender to palpation along the lateral joint line and has an effusion. They are tender to palpation along the medial and lateral facets of the patella. They have crepitus of the patellofemoral joint with range of motion and discomfort with patella grind testing.
The patient has no discomfort with McMurray’s maneuvers, and the knee is stable. They have limited range of motion. There are no erythema, warmth or skin lesions present.
An MRI result was presented during her follow-up visit and it showed Osteoarthrosis with high-grade cartilage loss in the medial compartment and high-grade cartilage loss central trochlear cartilage with low-grade chondral loss patellar cartilage.
Subchondral cystic changes and edema in the medial tibia are seen. This may be secondary to osteoarthritis although I cannot exclude developing insufficiency fracture medial tibia.
Large radial tear posterior horn medial meniscus which is peripherally extruded. Pes anserine bursitis. Large knee joint effusion with loose intra-articular body.
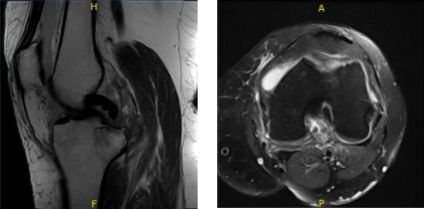
MRI-Left Knee Non-contrast
We discussed treatment options and opted for surgical management.
We discussed risks and benefits including infection, injury to adjacent nerves and vessels, pain in the knee, chronic pain, complex regional pain syndrome, need for repeat surgery, need for cortisones in the future, need for knee replacement in the future, systemic complications like deep vein thrombosis, cardiac, pulmonary, and neurological complications among others.
The patient understood and signed her informed consent.
The patient was taken to the operating room where general anesthesia was induced. She was placed on a well-padded operating table. IV antibiotics were given. The left lower extremity was prepped and draped aseptically in the usual fashion. A low tourniquet was applied. The tourniquet was inflated.
A lateral entry portal was made, and the scope was entered. A tear of the posterior horn of the medial meniscus was found. A medial entry portal was made. The probe was inserted, and the tear was re-examined. It was found to have a root avulsion of the posterior horn of the medial meniscus.
There was patellofemoral arthritis as well as medial femoral condyle arthritis. A decision was made to do the root repair. Chondroplasty of the patellofemoral arthritis which was grade 2 to grade 3 as well as the medial femoral condyle which was grade 3 to grade 4 was performed.
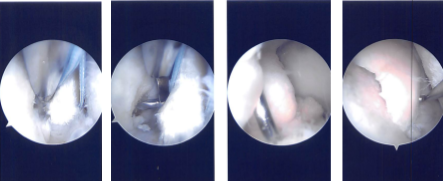
Intraoperative Arthroscopy Images
Curette was used to prepare the bed for the root. FiberWire #2 suture was passed through the root after preparation. Curette was used to prepare the bed by removing the articular cartilage as well as the bone. Scorpion was used to pass the sutures.
ACL zig was used to locate the site for the insertion of the root. Guiding through the ACL zig, an incision was given laterally onto the shin and the guide was inserted. A 2.5-mm drill bit was used to drill to the site of insertion. Finding it satisfactory, a suture retriever was inserted.
The sutures were passed through the suture retriever and retrieved out of the lateral shin of the tibia. Finding it in a satisfactory position on tightening, the sutures were tied over an EndoButton. The knee was irrigated thoroughly.
Closure was performed using #4-0 nylon. Then 30 cc of Naroin was injected into the knee. Dressing was done using 4 x 4, ABD, Webril, Ace wrap, and a knee immobilizer was applied. The patient was extubated and moved to recovery in stable condition.
The patient was informed to wear the knee immobilizer and to be weightbearing as tolerated with the knee in extension. She can remove the immobilizer and bend the knees up to 90 degrees without weight bearing. She is to use the walker for ambulation.
The patient was seen for post operative check up. We have decided to do formal physical therapy as well as a home exercise program for rehabilitation of the knee.
The patient regularly followed an office visit every 3-4 weeks. Patient did well after the surgery and continued physical therapy. Patient checked in for a follow up visit after a month and saw significant improvement on her knee.
Disclaimer – Patient’s name, age, sex, dates, events have been changed or modified to protect patient privacy.

Dr. Vedant Vaksha
I am Vedant Vaksha, Fellowship trained Spine, Sports and Arthroscopic Surgeon at Complete Orthopedics. I take care of patients with ailments of the neck, back, shoulder, knee, elbow and ankle. I personally approve this content and have written most of it myself.
Please take a look at my profile page and don't hesitate to come in and talk.
