Posterior Hip Replacement
Posterior hip replacement is the most common approach used for performing a total hip replacement. The approach is also known as southern or Moore’s approach is popular as it does not involve cutting of the abductor group of muscles.
The abductors help a person to walk without limping on taking a step. The approach also offers a good exposure of the thigh bone during the surgery as compared to the anterior approach.
Hip replacement is the most successful surgery in the entire history of medicine. Hip replacements today last for 20 years or even a lifetime. A total hip replacement may be performed for a number of reasons but arthritis of the hip remains the most common cause.
The arthritis of the hip may lead to painful movements about the hip joint during walking, sitting, driving, etc. A hip replacement surgery recreates the motion of the natural joint by replacing the diseased parts with prosthetic parts.
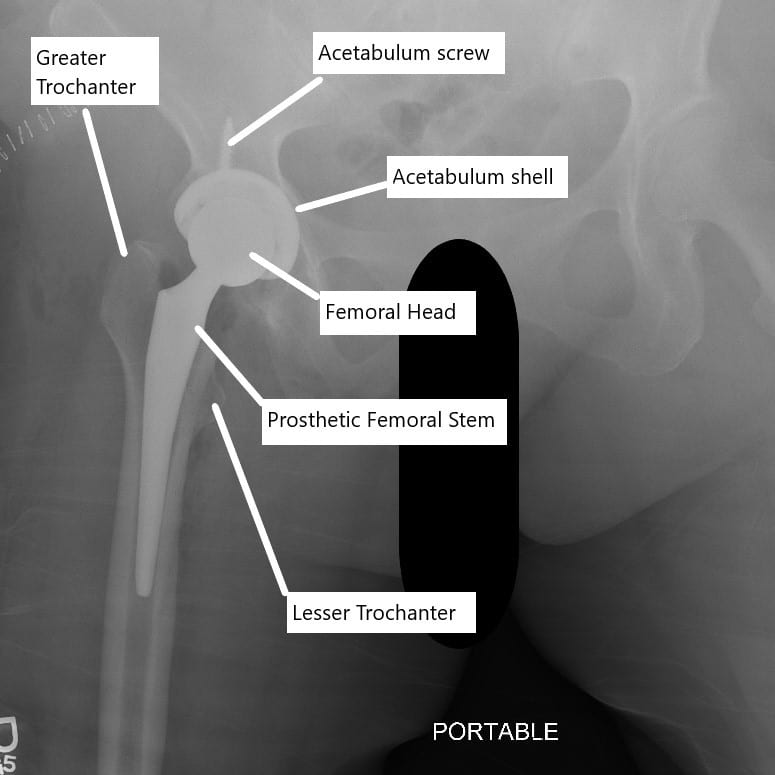
X-ray showing total hip replacement.
Approaches
During the surgery, the surgeon gives a skin incision followed by cutting or separation of the tissue to reach the hip joint. The hip joint may be accessed through a number of different approaches. In the posterior approach, the surgeon accessed the hip joint through the back of the joint.
Similarly in the anterior approach, the surgeon accesses the joint from the front. Other less commonly used approaches are the anterolateral and lateral approaches. The hip joint is accessed from the side in the direct lateral approach and if the incision is made some distance from the side to the front, it is known as the anterolateral approach.
The choice of surgical approach is often dependent upon a number of factors. Any prior incision, the selection of the implant, the risk of dislocation, obesity, hip deformity, and surgeon training all influence the choice of hip replacement approach.
Posterior approach
The surgery is usually performed under general anesthesia or at times may be performed under spinal anesthesia. The surgeon positions the patient on their side with the affected hip facing up. The surgeon may bend the hip and the knee of the affected side with the other leg laying straight.
After cleaning and draping in the usual fashion, the surgeon gives an incision in the back of the buttock in mimicking the alphabet “J”. The surgeon separates and cuts the underlying tissue known as fascia. The fascia is a tough tissue that covers the muscles.
Next, the surgeon separates the major muscle forming the buttock known as the gluteus maximus. The surgeon separates the muscle while taking care not to disrupt the blood supply and the nerve supply of the muscle. The trochanteric bursae are cleared in the operative field.
The affected side is manipulated in a position in order to rotate the hip inward. The inward rotating action places the small external rotator muscles in tension so the surgeon can see them clearly. The short external rotator muscles attach behind the upper part of the thigh bone. The muscles help in moving the hip outward.
Two of the short external rotator muscles piriformis and the obturator internus muscles are tagged and cut just near the upper thigh bone. During the process, the surgeon also takes care to locate the sciatic nerve to prevent inadvertent injury.
The hip capsule is a tough tissue that surrounds the hip joint. The tissue is cut using a special “T” shaped incision. The surgeon is now able to see the diseased joint and the surgeon cuts the neck of the thigh bone (femur) to separate the head of the femur from the upper thigh bone.
The head of the thigh bone is removed from the bony socket (acetabulum) using a special instrument. The cutting of the neck with a bone saw is done keeping in mind the implant position. The surgeon then proceeds to remove osteophytes also known as bone spurs around the socket.
The acetabulum socket is freshened with help of a reamer. The freshening of the bone in the socket helps the bone to grow on and in the acetabulum implant (cup). The reaming of the acetabulum socket is done in a position that allows maximum movement of the joint while maintaining stability. The prosthetic cup is press-fitted and may be additionally fixed to the acetabulum using screws.
The surgeon then uses a drilling instrument to locate the canal of the upper thigh bone. Rasping instruments in the shape of the implant are then inserted and removed with a larger size each time. The rasps and broaches help to freshen the canal of the thigh bone and prepare the seat for the implant.

Intraoperative image showing posterior hip replacement.
The last broach is left in place and the surgeon covers the neck of the trial broach with a trial head of the femur. The trail head is placed back in the socket using a maneuver and the surgeon checks for stability, range of motion, and length of the extremity.
Upon satisfaction with the size of the trial implants, the surgeon inserts the prosthetic femoral stem in the prepared upper thigh bone. The stem is press-fitted in the canal with a special emphasis on the direction and the angle of the final position. The stem is mostly press-fitted but may be fixed with bone cement in limited cases.
A prosthetic head made of metal alloy or ceramic is placed upon the neck. The metallic acetabulum socket is covered with a high-grade plastic liner. The head is placed back in the socket. The capsule as well as the cut short external rotators are repaired. The incision is closed in layers and a bandage is placed on the skin incision.
The patients are placed on deep vein thrombosis precaution in the form of blood-thinning medication such as aspirin. The patients are able to stand up and walk with assistance the next day of the surgery. The majority of the patients are able to walk without assistance (calipers/walkers) at the end of 3-4 weeks.
As with any surgery, there may be potential complications in the form of heart attack, blood clots, infection, bleeding, failure of hardware, leg length discrepancy, etc. Although rare, the complications are discussed at length with all patients undergoing hip replacement surgery. Hip replacement surgery has been a boon to millions of patients suffering from hip pain worldwide and is one of the most common surgeries performed by orthopedic surgeons.
Do you have more questions?
How does a PCL injury affect knee stability?
A PCL injury can significantly compromise knee stability, as the ligament plays a critical role in controlling the backward movement of the tibia under the femur.
How does posterior hip replacement differ from other approaches?
Unlike anterior or lateral approaches, posterior hip replacement involves accessing the hip joint through the back of the hip, allowing for exposure and placement of the prosthetic components.
What types of hip conditions or injuries are commonly treated with posterior hip replacement?
Posterior hip replacement is often used to treat conditions such as osteoarthritis, rheumatoid arthritis, avascular necrosis, hip fractures, and other degenerative hip disorders.
How is posterior hip replacement surgery performed?
During posterior hip replacement surgery, an incision is made at the back of the hip, and the damaged portions of the hip joint are removed and replaced with prosthetic components, including a metal stem inserted into the femur, a metal or ceramic ball attached to the stem, and a socket implanted in the acetabulum.
What are the benefits of posterior hip replacement?
Posterior hip replacement offers advantages such as excellent exposure of the hip joint, familiar surgical technique for many orthopedic surgeons, and good long-term outcomes in terms of pain relief and improved function.
What are the potential risks or complications associated with posterior hip replacement?
Risks and complications of posterior hip replacement may include infection, blood clots, dislocation of the prosthetic hip joint, nerve or blood vessel injury, leg length inequality, implant loosening, and the need for revision surgery.
How does the recovery process differ for posterior hip replacement compared to other approaches?
Recovery after posterior hip replacement may involve specific precautions to prevent hip dislocation, such as avoiding certain movements and positions during the initial healing phase. Physical therapy and rehabilitation are also essential components of the recovery process.
What factors determine whether a patient is a suitable candidate for posterior hip replacement?
Patient factors such as overall health, age, bone quality, hip joint anatomy, and the presence of any pre-existing medical conditions influence the decision to undergo posterior hip replacement surgery.
Are there any restrictions on physical activities or movements after posterior hip replacement surgery?
Patients may need to avoid certain movements and activities that place excessive stress on the hip joint, especially during the early stages of recovery. However, most individuals can gradually resume normal activities as tolerated with guidance from their healthcare provider.
How long does it take to fully recover from posterior hip replacement surgery?
The timeline for full recovery after posterior hip replacement varies depending on factors such as the patient’s age, overall health, adherence to post-operative instructions, and the extent of hip joint damage. However, many patients experience significant improvement within several weeks to months after surgery.
What are the potential long-term outcomes of posterior hip replacement?
Long-term outcomes of posterior hip replacement surgery may include pain relief, improved hip function, increased mobility, and enhanced quality of life for many patients. However, individual results may vary depending on factors such as patient age, activity level, and overall health.
What is the typical lifespan of prosthetic components used in posterior hip replacement?
The lifespan of prosthetic components used in posterior hip replacement varies depending on factors such as patient age, activity level, implant type, and implant material. In general, modern prosthetic components are designed to last 15-20 years or more with proper care and regular follow-up.
How does the risk of nerve injury differ between posterior hip replacement and other approaches?
Posterior hip replacement carries a risk of injury to the sciatic nerve, which runs close to the surgical site. However, advances in surgical technique and intraoperative monitoring have reduced the incidence of nerve injury in recent years.
What are the factors that influence the choice between posterior hip replacement and other surgical approaches?
Factors such as surgeon expertise, patient anatomy, hip joint pathology, patient preferences, and the presence of any pre-existing conditions or surgical risk factors influence the choice of surgical approach for hip replacement.
How does the risk of blood loss differ between posterior hip replacement and other approaches?
Posterior hip replacement may be associated with a slightly higher risk of blood loss compared to anterior or lateral approaches due to the larger incision and potential disruption of more soft tissue structures. However, transfusion rates are typically low with modern surgical techniques and blood conservation strategies.
Can posterior hip replacement be performed in patients with pre-existing medical conditions?
Posterior hip replacement may be performed in patients with certain pre-existing medical conditions, depending on the severity and stability of the conditions and the overall surgical risk. However, careful pre-operative evaluation and optimization may be necessary to minimize the risk of complications.
How does the risk of implant loosening differ between posterior hip replacement and other approaches?
Posterior hip replacement may be associated with a slightly higher risk of implant loosening compared to anterior or lateral approaches, particularly in patients with poor bone quality or suboptimal implant positioning. However, advances in implant design and surgical technique have improved implant stability and longevity in recent years.
Are there any specific post-operative precautions or instructions for patients undergoing posterior hip replacement?
Yes, patients undergoing posterior hip replacement surgery may receive specific post-operative precautions to minimize the risk of hip dislocation, such as avoiding crossing the legs, bending the hip beyond a certain angle, or sitting on low chairs or sofas. Compliance with these precautions is essential for successful recovery.
How does the risk of leg length inequality differ between posterior hip replacement and other approaches?
Posterior hip replacement may be associated with a slightly higher risk of leg length inequality compared to other approaches, as precise restoration of leg length and alignment may be more challenging due to the posterior surgical approach. However, careful pre-operative planning and intraoperative techniques can help minimize this risk.
Can posterior hip replacement be performed using robotic-assisted techniques?
Yes, posterior hip replacement surgery can be performed using robotic-assisted techniques, which offer potential benefits such as improved accuracy in implant placement, enhanced surgical precision, and better patient outcomes. Robotic technology may be particularly useful in cases involving complex hip anatomy or revision surgery.
How does the risk of infection differ between posterior hip replacement and other approaches?
Posterior hip replacement carries a risk of surgical site infection similar to other surgical approaches, although infection rates are typically low with modern surgical techniques and perioperative antibiotic prophylaxis. However, patient-specific factors such as immunocompromised status or obesity may increase the risk of infection in some cases.
Can posterior hip replacement be performed in patients with previous hip surgeries or revisions?
Yes, posterior hip replacement surgery can be performed in patients with a history of previous hip surgeries or revisions, depending on the specific circumstances and the underlying hip pathology. However, careful pre-operative evaluation and surgical planning are essential to address any anatomical challenges or complications from prior surgeries.
How does the risk of perioperative complications differ between posterior hip replacement and other approaches?
Posterior hip replacement may be associated with a slightly higher risk of certain perioperative complications such as nerve injury, wound healing problems, and blood loss compared to other approaches. However, careful patient selection, meticulous surgical technique, and adherence to evidence-based practices can help minimize the risk of complications in all approaches.
Are there any specific intraoperative considerations or techniques used in posterior hip replacement surgery?
Yes, posterior hip replacement surgery requires careful soft tissue dissection and retraction to access the hip joint from the back. Intraoperative techniques such as capsular repair, femoral head osteotomy, and acetabular reaming may be used to optimize implant placement and stability.
How does the risk of dislocation differ between posterior hip replacement and other approaches?
Posterior hip replacement may be associated with a slightly higher risk of hip dislocation compared to anterior or lateral approaches due to the posterior soft tissue structures being disrupted during surgery. However, careful surgical technique, appropriate implant selection, and patient education can help minimize this risk.
Can posterior hip replacement be performed using tissue-sparing approaches such as muscle-sparing techniques?
Yes, posterior hip replacement surgery can be performed using tissue-sparing techniques, which aim to minimize soft tissue damage, reduce post-operative pain, and accelerate recovery. These techniques typically involve smaller incisions and less disruption to surrounding muscles and tendons.

Dr. Suhirad Khokhar
My name is Dr. Suhirad Khokhar, and am an orthopaedic surgeon. I completed my MBBS (Bachelor of Medicine & Bachelor of Surgery) at Govt. Medical College, Patiala, India.
I specialize in musculoskeletal disorders and their management, and have personally approved of and written this content.
My profile page has all of my educational information, work experience, and all the pages on this site that I've contributed to.
