Case Study: Medial Meniscal Repair and Chondroplasty
of the Right Knee in a 50-year-old male
The patient is a 50-year-old male, with complaints of right knee pain, more for the last 3 months. The patient remembers injury to the right knee in a motor vehicle accident about a week before the onset of the symptoms.
The pain is extremely severe in intensity. The patient describes the pain as sharp. The pain is constant and does disturb sleep. The problem is associated with swelling, locking, weakness, and inability to straighten the knee. She is using an axillary crutch for ambulation.
The pain is not associated with bruising, instability, or giving way, crepitus, tingling, numbness, radiating pain, weakness, gait, or bowel or bladder abnormality. The problem has been getting worse since it started. Standing, twisting, bending, squatting, kneeling and stairs make the symptoms worse. Rest and elevation make the symptoms better.
The patient does not smoke or use recreational drugs. The patient is on Gabapentin 300mg and Tizanidine 4mg. He denies any other medical condition and denies any known drug allergies.
On examination, the patient is calm conscious cooperative, and well oriented to time place and person. The patient walks with an assistive device in the form of axillary crutches. Upon examination of the right knee, the patient is tender to palpation along the medial joint line and has an effusion.
The patient also has patellofemoral crepitus and tenderness on palpation along the medial and lateral PF joint line. The patellar grinding test is positive. The patient has discomfort with McMurray’s maneuvers, and the knee is stable. The right knee lacks full flexion secondary to the effusion but has a full extension. Both the lower extremities have 5/5 strength and are neurovascularly intact distally. There are no erythema, warmth, or skin lesions present.
On examination of the contralateral extremity, the patient is non-tender to palpation and has an excellent range of motion, stability, and strength.
X-Ray of the right knee suggested mild osteoarthrosis in the medial and anterior compartment of the knee.


MRI of the right knee suggested medial meniscus tear and patellofemoral arthritis of the right knee.

Various treatment options, risks, and benefits of the surgical and nonsurgical treatment, the patient opted for surgery and informed consent was signed. The patient was informed regarding the possibility of meniscal repair, and in case of meniscal repair, she will be needed to use leg brace crutches and a brace and ambulate with the knee straight only. We discussed the postoperative rehabilitation and protocol.
The patient was taken to the operating room and placed on a well-padded operating table. General anesthesia was induced. A tourniquet was applied over the right lower extremity. The right lower extremity was prepped and draped aseptically.
Esmarch was applied, and the tourniquet was elevated to 300 mmHg. Tourniquet time was 59 minutes. A time-out was called.
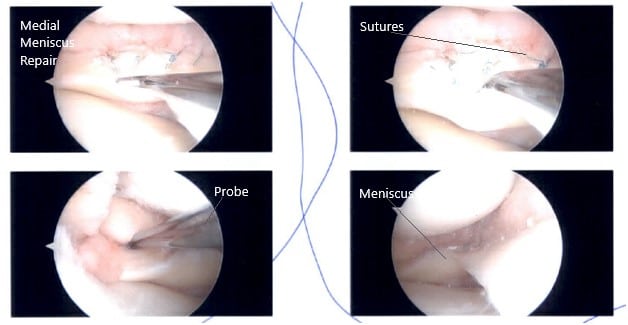
A lateral entry portal was established, and the knee joint was examined. A peripheral tear of the medial meniscus was found. A grade 1 to grade 2 osteochondral lesion of the medial condyle of the femur was also found. The ACL had some fraying and degeneration.
There was no lesion on the meniscus or lateral femur and condyle. The patellofemoral joint was inspected and found to be good. Now, the repair of the medial meniscus was performed. FasT-Fix sutures were used. Seven sutures were used to fix the peripheral tear from the posterior horn to the midbody.
Gross fixation and stability of the meniscus was found to be satisfactory. Final arthroscopic pictures were taken. The knee was lavaged with copious normal saline. The wound was closed
using nylon #4-0. The dressing was done using 4 x 4s, Webril, and Ace wrap.
The patient was extubated and moved to the holding area in a stable condition. The postoperative examination of the distal pulses and neurological status was intact.
Disclaimer – Patient’s name, age, sex, dates, events have been changed or modified to protect patient privacy.

Dr. Suhirad Khokhar
My name is Dr. Suhirad Khokhar, and am an orthopaedic surgeon. I completed my MBBS (Bachelor of Medicine & Bachelor of Surgery) at Govt. Medical College, Patiala, India.
I specialize in musculoskeletal disorders and their management, and have personally approved of and written this content.
My profile page has all of my educational information, work experience, and all the pages on this site that I've contributed to.
