Case Study: Meniscal Repair of the Medial Meniscus
on the left knee of a 25-year-old male
Meniscus safeguard the bones from the enormous pressures that pass through the knee joint as we move. As a result, the bones have a smooth surface that facilitates motion.
During abrupt knee twists, such as those that occur during sports or falls, the menisci are frequently damaged. As a result, the joint may enlarge and bleeding may occur, which tends to tear some of the cartilage.
In contact sports, meniscus injuries are prevalent; frequently they co-occur with ligament injuries, especially when the medial meniscus is affected. This is partially due to the fact that the medial meniscus is connected to the medial collateral ligament and partially because tackles are frequently made to the lateral side of the knee, which causes the tibia to externally rotate.
Injury in medial meniscus is associated with knee discomfort, swelling, and locking, which occurs when the patient is unable to fully straighten the leg. A clicking sensation could also accompany this.
A 25-year-old male patient visited our office, with complaints of left knee pain which he got a few months ago. The patient was playing soccer and the pain started. The pain got better over time, but he re injured again and has been having pain since then. The pain is intermittent and does disturb sleep.
The pain is associated with bruising but is not associated with swelling, tingling, numbness, radiating pain, weakness, bowel or bladder abnormality, gait problem, giving way, or limping, hand function difficulty.
The problem has been getting worse since it started. Moreover, the patient is a smoker. With the help of physical therapy it makes the symptoms better. Patient is currently taking Advil.
Upon examination of the left knee, the patient is tender to palpation along the medial joint line and has an effusion. The patient has discomfort with McMurray’s maneuvers, and the knee is stable. They lack full flexion secondary to the effusion but have full extension.
There are no erythema, warmth or skin lesions present. On examination of the contralateral extremity, the patient is nontender to palpation and has excellent range of motion, stability, and strength.

Left Knee X-ray AP and Lateral with Obliques 3 views
X-ray results were presented during the visit and showed no significant degenerative changes. There are no acute fractures. There is no fracture, subluxation, or dislocation. No osteoblastic or osteolytic lesions can be identified. The joint spaces are preserved. The subarticular cortex is smooth. A joint effusion is demonstrated.
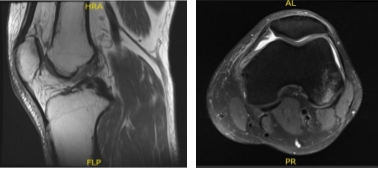
MRI – 3T Left Knee Non Contrast
MRI result was presented today and shown complex tear of the posterior horn of the medial meniscus, small horizontal cleavage tear of the body of the lateral meniscus, impaction injury of the posterior non weight bearing aspect of the lateral femoral condyle with small fracture,
Grade 2 medial collateral ligament injury with vertical longitudinal tear, Contusion in the inferior medial aspect of the patella, Moderate joint effusion with synovitis.
We discussed the treatment options for the patient’s diagnosis, which included living with the extremity as it is, organized exercises, medicines, injections and surgical options. We also discussed the nature and purpose of the treatment options along with the expected risks and benefits.
I educated the patient regarding the inherent and unavoidable risks which include, but are not limited to: anesthesia, infection, damage to nerves and blood vessels, blood loss, blood clots, and even death were discussed at length.
We talked about the possibility of not being able to return to prior activities or employment, the need for future surgery, and complex regional pain syndrome and understands there is a long rehabilitative process that typically follows the surgical procedure.
Also explained that there is no guarantee all the function and strength will return. The patient also understands the risks of re-tear or failure to heal. The patient expressed understanding of these risks and has elected to proceed with surgery.
We also discussed repair vs debridement of the medial meniscus. Patient’s quitting smoking is paramount to successful treatment. We also discussed the possibility of ACL tear and repair vs reconstruction of ACL. Patient declined to undergo ACL reconstruction but was ready for an ACL repair if needed.
The patient was taken to the operating room and placed on a well-padded operating table. General anesthesia was induced. The left lower extremity was put in a tourniquet. It was prepped and draped aseptically in a usual fashion. The left thigh was put into a knee holder. Preoperative antibiotic was given.
Esmarch was applied and the tourniquet was inflated to 300 mmHg. Patellofemoral joint was found to be in good shape with no cartilage damage. The scope was taken to the medial gutter where there was a synovial flap. Medial compartment showed a ramp lesion of the posterior body of the medial meniscus.
Probe was inserted and meniscus tear was again checked. It involved the posterior body of the medial meniscus along the capsule. The decision was made to repair the ramp lesion using all-inside suture configuration using FasT-Fix.
Two curved and two reverse curved FasT-Fixes were used to complete the repair after the meniscus was abraded along with a capsule abrasion done with the shaver. The repair was found to be in good position.
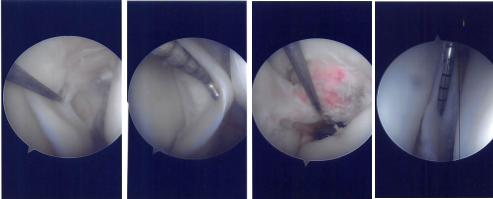
Intraoperative Arthroscopy Images
Now the scope was moved to the internal trochlear area where ACL was deficient. Debridement was done. The scope was moved to the lateral compartment where we found medial edge fraying as well as a small bucket handle tear of the medial edge of the lateral meniscus.
Further examination showed a horizontal tear going up to the periphery of the lateral meniscus of the posterior body. Three FasT-Fixes were used for repair of the lateral meniscus, horizontal lesion.
Before that, posterolateral incision was given anterior to the fibula. With sharp and blunt dissection making a plane behind the LCL and between the knee capsule in the lateral head of gastrocnemius, a plane was made.
Sims speculum was inserted to protect the posterior neurovascular bundles. After it was done, the scope was reentered and the repair of the left meniscus using FasT-Fixes were done in a satisfactory fashion. Microfracture of the trochlear notch was performed using bundle fix.
The tourniquet was released, and bleeding bone could be seen from the microfracture site. The posterolateral wound Incision was washed and closed. Hemostasis was achieved. Closure was done in layers. The posterolateral incision was closed with Monocryl. The arthroscopic portals were closed using nylon.
Dressing was applied. The knee was put in a knee mobilizer. The patient was extubated and moved to the postoperative care unit in a good condition.
We have decided to proceed with formal physical therapy as well as a home exercise program for rehabilitation of the knee. Stitches were removed during today’s visit.
We will continue with ice and elevation of the knee to decrease swelling and pain and will also continue to utilize early mobilization and mechanical prophylaxis to reduce the chances of a deep vein thrombosis.
We will wean them off any narcotic medications and progress to anti-inflammatory and Tylenol if there are no contraindications to these medications. Patient checked in for a follow up visit after a few weeks and saw significant improvement on his knee.
Disclaimer – Patient’s name, age, sex, dates, events have been changed or modified to protect patient privacy.

Dr. Vedant Vaksha
I am Vedant Vaksha, Fellowship trained Spine, Sports and Arthroscopic Surgeon at Complete Orthopedics. I take care of patients with ailments of the neck, back, shoulder, knee, elbow and ankle. I personally approve this content and have written most of it myself.
Please take a look at my profile page and don't hesitate to come in and talk.
