Case Study: Right Total Hip Arthroplasty
in a 45 year-old patient
A total hip replacement, also known as a total hip arthroplasty, involves the removal of the diseased bone and cartilage and its replacement with artificial parts. A metal stem is inserted into the hollow middle of the femur to replace the broken femoral head.
Hip strains happen when one of the muscles that supports the hip joint is overextended or damaged. In accordance with the severity of the damage, strains might range from minor to severe. A significant strain may restrict your hip’s range of motion.
Patient visited our office with complaints regarding bilateral hip pain. Left hip improved but the right hip has worsened despite use of stretching exercises and NSAIDs. She is limping and is not able to be fully functional the whole day due to pain.
For associated symptoms, patient reported no weakness, no numbness, no tingling, no swelling, no redness, no warmth, no ecchymosis, no catching/locking, no popping/clicking, no buckling, no grinding, no instability, no radiation, no drainage, no fever, no chills, no weight loss, no change in bowel/bladder habits, and no tenderness.
She presented MRI results for both of her hips that showed mild common hamstring tendinosis with a small intrasubstance tear and surrounding edema at the ischial tuberosity. Extensive avascular necrosis of the right femoral head. Degenerative changes in the lower lumbar spine for her left hip.
Extensive avascular necrosis involving the majority of the right femoral head and surrounding bone marrow edema extending into the femoral neck. Crescentic subchondral fracture line is seen medially without articular collapse or fragmentation.
There are mild osteophytic changes of the right femoral acetabular joint and a moderate joint effusion. Mild gluteus minimus tendinosis without a tear, for the right hip.
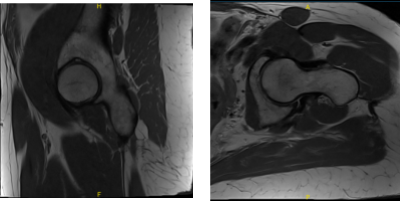
MRI Left hip non-contrast
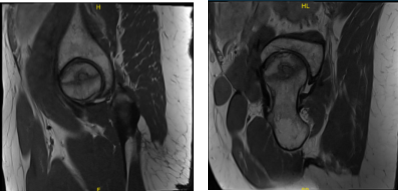
MRI Right hip non-contrast
We discussed the treatment options for the patient’s diagnosis, which included living with the extremity as it is, organized exercises, medicines, injections, and surgical options. We also discussed the nature and purpose of the treatment options along with the expected risks and benefits.
I educated the patient regarding the inherent and unavoidable risks which include, but are not limited to anesthesia, infection, damage to nerves and blood vessels, blood loss, blood clots, and even death were discussed at length.
We also talked about the possibility of not being able to return to prior activities or employment, the need for future surgery, and complex regional pain syndrome. The patient also understands there is a long rehabilitative process that typically follows the surgical procedure.
We talked about the possibility of not being able to alleviate all of the discomfort. Also, I explained there is no guarantee all the function and strength will return. The patient also understands the risks of re-tear or failure to heal.
The patient expressed understanding of these risks and has elected to proceed with surgery. We have discussed the surgical procedure as well as the realistic expectations regarding the risks, outcome, and post operative protocol.
The patient was brought to the operating room after obtaining informed consent and signing the correct surgical site. The risks, benefits, and alternatives were extensively discussed with the patient prior to the procedure.
The patient understands increased risk of young age and that she might need a revision in the future. Anesthesia was obtained by the anesthesiologist. The patient was then definitively positioned with the right hip up and the right hip was then draped and prepped from the usual sterile manner.
A curved incision centered over the greater trochanter was used for the arthrotomy. Skin and subcutaneous tissues were incised. Fascia was then divided. The hip was then placed into internal rotation. The posterior soft tissue structures were then tacked and the hip was then dislocated.
The neck resection was then made at the correct level. The head was then removed. Attention was then turned towards the acetabulum. The acetabulum was debrided and reamed and the shell was placed into the acetabulum in the correct abduction and anteversion. The screw was used for additional fixation. The poly was then placed over the shell.
Attention was then turned towards the femur. The femur was then sequentially broached. The final broach was left into position. The trunnion and the head were then placed over the broach and the hip was then reduced.
The hip was then trialed through a full physiological range of motion and was found to be stable in all physiological ranges of motion. The combined version was found to be correct. The hip was then dislocated. The trial components were then removed. Final components were then placed into position and the hip was then relocated.
Thorough lavage was given. Injection was given. Posterior soft tissue structures were then tacked to the greater trochanter through transosseous tunnels. Thorough lavage was given. Fascia was closed with Ethibond. The closure was done by plastic surgeon, Dr. Kote.
The patient was given status post right total hip arthroplasty using zimmer, said she slept in her side ” by mistake” and felt hip dislocated. She presented an X Ray that showed right total hip arthroplasty, in good alignment. There are no fractures.
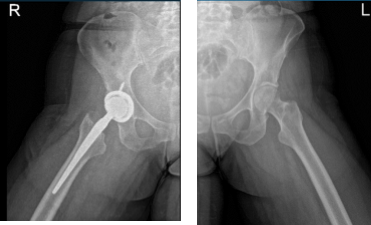
Hip Bilateral with pelvis 3 or 4 more view
The patient was seen for post operative check up. We have decided to do formal physical therapy as well as a home exercise program for rehabilitation of the hip.
Patient did well after the surgery and continued physical therapy. Patient checked in for a follow up visit after a month and saw significant improvement on her hips.
Disclaimer – Patient’s name, age, sex, dates, events have been changed or modified to protect patient privacy.

Dr. Vedant Vaksha
I am Vedant Vaksha, Fellowship trained Spine, Sports and Arthroscopic Surgeon at Complete Orthopedics. I take care of patients with ailments of the neck, back, shoulder, knee, elbow and ankle. I personally approve this content and have written most of it myself.
Please take a look at my profile page and don't hesitate to come in and talk.
