Case Study: Right Knee Arthroscopic Excision
in a 47-year-old patient
By using a surgical technique called a knee arthroscopy, surgeons may inspect the knee joint without having to make a significant incision (cut) through the skin and other soft tissues. A variety of knee issues are diagnosed and treated using arthroscopy.
Overuse, insufficient training, osteoporosis, and participation in high-impact sports involving abrupt changes in direction are risk factors for knee injuries. Knee pain and swelling are the primary warning signs and symptoms of knee damage.
A 47-year-old patient was in our office with complaints regarding right knee pain. The patient was skiing when he injured his knee. He went to City MD where x-rays were taken. The severity of the pain is 5/10.
The quality of the pain is constant, and he has swelling. The pain is less when it rests and applies ice. Walking aggravates the pain.
We discussed risks and benefits including infection, bleeding, injury to adjacent nerves and vessels, failure of healing, need for ACL reconstruction in the future, arthritis, and need for knee replacement in the future among others.
We discussed systemic complications Including blood clot, cardiac, pulmonary, neurological complications, among others. The patient understood and signed an informed consent.
The patient was taken to the operating room where a regional block was performed by the anesthesia team. General anesthesia was induced. Right lower extremity was prepped and draped aseptically in the usual fashion. Preoperative antibiotic was given. One gram of TXA was also given before surgery.
The tourniquet was elevated after exsanguinating the limb. Lateral entry portal was made. Arthroscope was inserted. Examination of the patellofemoral compartment showed no cartilage damage. Examination of the medial tibiofemoral compartment showed no meniscus or cartilage tear.
The Medical entry portal was made with the use of a spinal needle. Examination of the anterior patellar notch showed that avulsion of the ACL from the tibial attachment with raw bone. It was thoroughly irrigated and drained.
Examination of the lateral tibiofemoral compartment showed tearing of the anterior horn of the lateral meniscus in line with the ACL along with the intermeniscal ligament. It was decided not to repair the lateral meniscus because it was falling in line once the reduction of the ACL fragment was done.
The ACL fragment was reduced in its place and held with the use of a tibial tray. A #2 FiberTape was passed with the use of labral Scorpion through the posterior fibers of the distal ACL. This was followed by passage of a 1.3 mm Suture Tape in the same vicinity to achieve good hold on the ACL ligament.
The fragment was again held with the tibial ACL ring and a Beath pin was passed through the separate incision distally from the tibia into the knee joint. The sleeve was removed, but the ACL ring was kept in place to keep the fragment in place. A 4-mm cannulated drill was passed over the Beath pin and the Beath pin was removed.
Now, suture passer was passed through the cannulated drill and the cannulated drill was removed. The four tails of the sutures were noted on to the suture retrieval lasso and passed out of the tunnel. Once they were out, a good reduction of the ACL could be seen. There was no laxity of ACL.
All the four tails of the suture were put into the tibia with the use of 4.75 SwiveLock after drilling and tapping. A good reduction was achieved Final picture was taken and saved.
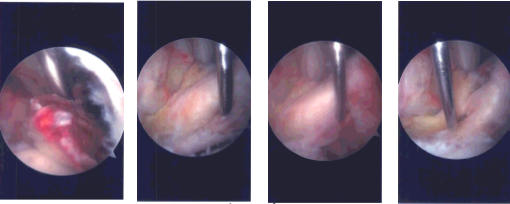
Intraoperative Arthroscopy Images
The anterior horn of lateral meniscus was found to be well reduced. The knee was thoroughly irrigated and drained. Closure was done with the use of #3-0 nylon. Dressing was done with the use of Xeroform, 4 x 4, ABD, Webril and Ace wrap. A knee immobilizer was applied after the surgery. The patient was extubated and moved to recovery in a stable condition.
The patient was seen for post op follow up checkup and he still has pain. He got a CT scan done of his knee. It showed status post comminuted fracture of ACL footprint and postsurgical reimplantation of PCL attached to the largest fracture fragment. No evidence for bony union is evident.
No interval change is seen in the position of the large and small fragments. There is a thickened appearance of the ACL outlined. No interval changes in the appearance of tiny fracture fragments peripheral to medial condyle, peripheral to lateral tibial plateau and slight residual osteochondral irregularity of peripheral posterior lateral plateau.
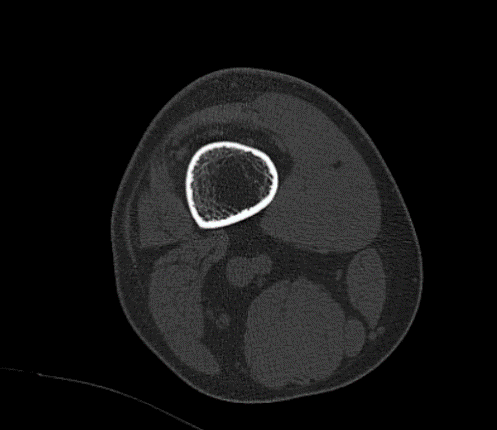
CT-Right Knee Non-contrast
The patient undergoes a surgery again for revision, arthroscopic in knee. The patient was taken to the operating room. Adductor canal block was given. General anesthesia was induced. The right hip and right knee were prepared aseptically in the usual fashion after application of a tourniquet.
About with the help of draping and Ioban. The right knee was prepped for arthroscopy. Initial incision was given over the right iliac crest. a 3 cm incision was given about 3 cm posterior to the dissection. The periosteum was cut in the line of incision.
Periosteum elevator was used to elevate the periosteum from the medial and lateral surface of the iliac crest. High-speed oscillating saw was used to cut a lateral block of about 1.5 cm wide in a form of wound flap which was opened up.
Curette was used to take out about 1.5 cc of cancellous wound from the iliac crest. The wound was thoroughly irrigated and drained. The flap was put back and the periosteum was sutured. The closure was done with the use of #0 Vicryl, #2-0 Vicryl and #3-0 Monocryl.
The attention was focused onto the right knee. The wound VAC was kept in a saturated Ray-Tec. A lateral entry portal was made towards the right knee for laparoscopic viewing. The scope was entered. A medial entry port was made with the use of a spiral needle.
A Crosswood cannula was put on the medical entry portal. Examination of the knee showed intact medial and lateral compartments of use of 7 cc of 0.25% Marcaine was done in the right hip region with local anesthesia.
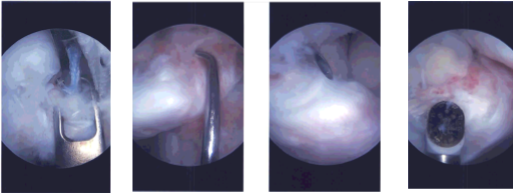
Intraoperative Arthroscopy Images
There was an intact patellofemoral compartment. In the intercondylar notch there could be seen a free fragment from the distal ACL. It was all covered in fibrosis and was held in pieces with the fibrotic tissue. Shaver was used through the debridement.
This was followed by 4.5 mm to decorticate the tibial portion. The femoral portion was decorticated with the use of a shaver so as not to deep off excess bone from there. The ACL was reduced and held in place with an ACL jig and a K-wire was passed to temporarily hold it.
Two intraosseous tunnels were made, one medial and one lateral to be passed and secured. Now, the ACL footprint is used to pass FiberTape x2 through the ACL distal stump. This was passed into the intraosseous tunnel to see the reduction.
The reduction was not appropriate so the lateral lens of the FiberTape was also taken out from the medial intraosseous tunnel and a good reduction could be seen. Once we were able to get a good reduction, lateral parapatellar transverse incision was given to do a mini arthrotomy.
After the reduction, the fracture site could be seen and was inserted into the fracture site and was found to be in acceptable position. This was followed by tightening and knotting of the fiber kits over EndoButton. Arthroscope reduction with a SwiveLock after drilling 5.25 and insertion of 4.75 SwiveLock.
Knee dressing was done with the use of Steri-Strips, 4 x 4’s and Tegaderm. an immobilizer was applied in extension over the right knee. The patient was extubated and moved to recover in a stable condition.
The patient was seen for post op follow up checkup and showed healing in the posterior and medial part of the fracture. He was scheduled to present a CT scan of the knee.
We have decided to do formal physical therapy as well as a home exercise program for rehabilitation of the knee. Patient checked in for a follow up visit after a month and saw significant improvement on his knee.
Disclaimer – Patient’s name, age, sex, dates, events have been changed or modified to protect patient privacy.

Dr. Vedant Vaksha
I am Vedant Vaksha, Fellowship trained Spine, Sports and Arthroscopic Surgeon at Complete Orthopedics. I take care of patients with ailments of the neck, back, shoulder, knee, elbow and ankle. I personally approve this content and have written most of it myself.
Please take a look at my profile page and don't hesitate to come in and talk.
