Case Study: Open Reduction Internal Fixation:
Closed Fracture of Patella in a 73 year-old woman
If the patella pieces do not enter the skin, a kneecap fracture is regarded as closed. Open kneecap fractures result in complex wounds because the bones protrude through the skin. The majority of patella fractures are closed fractures, meaning that the patella does not penetrate the skin.
The patient, a 73 year-old woman, was diagnosed with an displaced fracture of the patella on the right side after the doctor examined her about a month ago. She received conservative care while wearing a knee brace.
She put a lot of effort into her home, especially during the flooding, and in the process she dislodged the patella fracture. When I saw her again in my office, we discovered that she had a dislocated patella fracture.
We discussed treatment options and opted for surgical management. She had uncontrolled hypertension and had not seen her primary care doctor in years. She was asked to get medical care, which took us about three weeks in the process. Once it was done, she was scheduled for surgery.
We discussed the risks, benefits and complications of the surgery including infection, bleeding, injury to adjunct nerves and blood vessels, failure, need for repeat surgery, need for rehabilitation, arthritis and the need for implant removal and knee replacement in future, systemic complications including blood clot, cardiac and pulmonary complications including death. The patient understood and signed the informed consent.
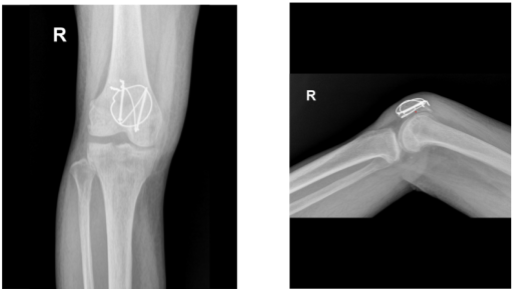
X-ray Image right knee
The patient was brought into the operating room and laid out on a sturdy operating table. Anesthesia was induced throughout. The tourniquet was wrapped around the thigh. The right lower extremity was prepared as normal and dressed aseptically. A break was announced.
An antibiotic was given before surgery. From 2 cm proximal to 2 cm distal to the patella, a longitudinal incision was made, centered over the patella. Sharp dissection allowed exposure to penetrate all the way to the bone. A break was made.
Opening the fracture site allowed for full irrigation. A thorough irrigation was performed after the knee arthrotome. Up to the quadriceps tendon and patellar tendon on either side, the patella’s periosteum was visible. Using a curette, the fracture was thoroughly cleaned.
The fracture received a thorough irrigation. The fracture was reduced and secured with a clamp. After creating a short vertical incision to the patellar tendon, two K-wires were transferred from the distal bone to the proximal bone once the fracture was securely stabilized. After measuring the K-wires, two cannulated cancellous screws were medially and laterally placed over the K-wires to accomplish fixation.
The anterior patellar surface was then perforated by making a figure-eight with an 18-gauge stainless steel wire after it had been threaded through the two screws. The wires were tied super laterally with a knot that was secured.
Due to osteoporosis, there was some comminution and the lateral screw was moved proximally by the wire. A cerclage wiring was applied to the 18-gauge wire once more to support the fixing. A satisfactory fixation was attained once the cerclage was finished and the knot was tightened super laterally.
The knee could be comfortably moved from 0 to 60 degrees. There was a thorough irrigation and drainage of the knee. After shrinkage with vancomycin, closure was done in layers. Vicryl 4-0 and 2-0 were used for the closure, along with staples.
With the aid of Xeroform, ABD, Webril, and Ace wrap, dressing was completed. A knee brace was put on. After being extubated, the patient was transferred to the recovery room in stable condition.
The patient went to the office for her postoperative visit with x-rays of her right knee. She is in a knee immobilizer, she denies fever and chills. She is ambulating with a brace locked in extension without aid.
After the examination we discussed treatment options including PT, MRI, Injection, surgery and we agreed to go with conservative management for now. Continue the use of knee immobilizer, locked in extension when OOB, gentle knee ROM 0-60 degree as tolerated, Ice/heat, Elevation and taking OTC anti-inflammatory meds. The patient follows up after 5 weeks, and may start PT at that time.
After one month from the surgery, the patient was discharged. She is doing outpatient PT and at home and she is gradually improving and the doctor advised her that she can visit the office as needed.
Disclaimer – Patient’s name, age, sex, dates, events have been changed or modified to protect patient privacy.

Dr. Vedant Vaksha
I am Vedant Vaksha, Fellowship trained Spine, Sports and Arthroscopic Surgeon at Complete Orthopedics. I take care of patients with ailments of the neck, back, shoulder, knee, elbow and ankle. I personally approve this content and have written most of it myself.
Please take a look at my profile page and don't hesitate to come in and talk.
