Case Study: ACL, Arthroscopic Assisted Reconstruction
with Autograft in a 33 year-old female
The injured ligament is restored in an ACL reconstruction with a tissue graft from a donor (allograft) or your own body (autograft).
Clinical outcomes with autografts are comparable to or slightly better than those with allografts in ACL restoration. Despite autograft’s ability to promote bone healing, it has a number of disadvantages.
Additional surgical procedures, greater infection risk, increased blood loss, limited amount, and donor-site hypersensitivity or morbidity are among them.
The patient is a 33 year-old female who has been seen in the office for almost six months. She was in a car accident and suffered from pain and edema in her left knee. An MRI revealed a full bucket handle medial meniscus tear into the intercondylar notch.
The patient has a 30-degree flexion deformity and is unable to extend. The patient has been limping for some time. We discussed the therapy choices with the patient, who chose surgical management. Due to social constraints, the patient has been unable to undergo surgery. The patient refuses surgical intervention.
We addressed the dangers and benefits, including infection, bleeding, damage to the nerves and blood vessels, the necessity for more surgery, and the need for rehabilitation. We talked about the potential for arthritis to develop in the future, the necessity for replacement, and other issues like blood clots, etc. The patient signed the consent after fully understanding it.
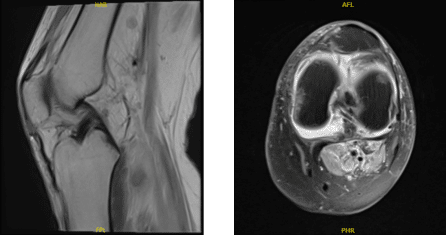
MRI-3T Left Knee non-contrast
The patient was brought to the surgery room. The anesthetic team administered a nerve block to the patient. A preoperative antibiotic was administered. Under anesthesia, the Lachman and anterior drawer tests were positive, while the pivot shift test was negative.
A high thigh tourniquet was administered, and the left lower extremity was prepped and draped aseptically in the usual manner using a clamp. A timeout has been called.
A midline suprapatellar incision was made to harvest the quadriceps tendon, and bony landmarks were delineated. The paratenon was detached from the incision line, and the tendon was cleansed and separated.
The tendon was marked for around 10 mm width and sliced on both sides with the blade before inserting the Arthrex bone graft harvester. A total of 70 mm of graft was extracted and sliced with a cigar cutter.
On the back table, the wound was packed, and the graft was prepared with Arthrex QuadLink using Fiber Tape and Fiber Wire with an adjustable EndoButton for the femoral side and the same preparation for the tibial side but no EndoButton.
The graft was stretched on the back table and measured to be 9 mm wide and 65 mm long after it was prepared. On the graft, markings were made. The transplant was encased with normal saline saturated with vancomycin. Esmarch was used, and the tourniquet was raised.
The lateral portal was used to implant the arthroscope. It revealed a tear in the capsule of the quadriceps tendon’s lateral side. It was intended to be closed, and a separate incision was made to do so.
The arthroscopy was restarted once this was completed. In the patellofemoral, medial, or lateral compartments, there were no osteoarthritic alterations. The ACL was not present.
The medial meniscus had a bucket handle rupture that was dangling in the intercondylar notch. A medial anterior portal was created, and the bucket handle rip was successfully reduced. It was decided to repair it from the inside out. To prepare the margins, a meniscus grasper was used.
Arthrex meniscal sutures were utilized three times to mend horizontal mattress sutures, and the repair was successful. Photographs were taken and preserved. The ACL was prioritized, and the medial surface of the lateral femoral condyle was prepared for ACL surgery.
The tibial plateau was similarly treated and marked with the ArthroCare wand. Another arthroscope was placed through the medial portal, followed by the insertion of a femoral jig and the insertion of a sleeve.
The skin was prepared to allow for the insertion of the sleeve, which was then hammered into the bone. The sleeve was cut with a flip cutter that was placed through the sleeve. Once within, the FlipCutter was deployed to 9.5 mm, and a 25 mm tunnel was created in the femoral side.
The FlipCutter was rotated back and drawn out, then the betrick was inserted, and the suture was tied into itself to maintain the canal patent. The arthroscope was now introduced through the lateral portal, a tibial jig through the medial portal, and the sleeve through a second incision on the medial shin.
Drill was inserted similarly and flipped once inside the joint to create a 9 mm x 25 mm tunnel. The drill was flipped back and removed once more. Suture through fiber stick was used to keep the canal patent.
The knee was extensively irrigated to remove any wound debris before being removed and drained. Both suture loops were removed through the same passageway on the medial side, and the medial portal was enlarged.
The quad tendon was extracted and placed first on the femoral side before being pulled out. The tibial end was likewise dragged out with the loop once it was inside the knee. The tendon was positioned according to its markings and tightened on both sides, the tibial side on an axial button.
The knee was then cycled 30 times in flexion and extension, the ligament was tightened on both sides, and the sutures were knotted together and snipped. The final images were stored and saved.
Acromioplasty was performed to eliminate an impingement on the lateral femoral condyle. As a result, there was no impingement. The final photographs were shot and preserved. The wound was irrigated and drained carefully.
The quad tendon harvest site was closed in layers with 0 Vicryl, 2-0 Vicryl, and Monocryl, and the arthroscopic incisions were closed with nylon. Dermabond, Telfa, 4×4, ABD, Webril, and Ace wrap were used for dressing. In addition, a knee immobilizer was used. In stable condition, the patient was extubated and sent to Recovery.
Rafael Robenov was present during the latter half of the surgery and was important in assisting with tendon insertion, fixation, tightness, hemostasis, and wound closure.
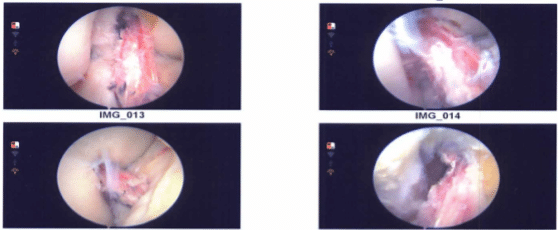
Intraoperative images
The patient seen in the office for her one week post operative visit, her pain is poorly controlled though better than before and She is using immobilizer and crutches also denies fever, chills.
We opted to proceed with official physical therapy as well as a home workout regimen for knee rehabilitation after examining treatment choices. During the visit, we reviewed the arthroscopy images and removed the stitches. We will continue to use ice and elevate the knee to reduce swelling and pain.
To limit the risk of deep vein thrombosis, we will continue to use early mobilization and mechanical prophylaxis. We will gradually wean them off any narcotic medications and transition them to anti-inflammatories and Tylenol as long as there are no contraindications.
We also covered the risks and benefits of taking these medications, as well as the most prevalent side effects. The patient will return in three weeks to assess their progress.
The patient visited the office for her postoperative visit, her pain had been well controlled and she was improving with ROM and weight bearing for almost a month when she had a fall at Burger king restaurant and she reinjured her left knee.
Her pain has been worsening since then and she is not able to extend her knee. She is using an immobilizer and crutches and denies fever or chills. We discussed treatment options including PT, MRI, Injection, surgery and we agreed to go with 3 Tesla MRI and PT to be started as discussed.
The patient is still making improvement, albeit slowly, with help of monthly examinations and physical treatment and at home.
Disclaimer – Patient’s name, age, sex, dates, events have been changed or modified to protect patient privacy.

Dr. Vedant Vaksha
I am Vedant Vaksha, Fellowship trained Spine, Sports and Arthroscopic Surgeon at Complete Orthopedics. I take care of patients with ailments of the neck, back, shoulder, knee, elbow and ankle. I personally approve this content and have written most of it myself.
Please take a look at my profile page and don't hesitate to come in and talk.
