Case Study: Knee Arthroscopy: Medial Meniscectomy
with Bone Biopsy and Debridement in a 28-year-old female
An arthroscopic procedure called a meniscectomy and debridement involves removing all or a portion of a damaged meniscus. Surgically removing loose bits of cartilage and bone from the joints is known as arthroscopic debridement. A damaged meniscus is removed using an arthroscopic procedure known as a meniscectomy.
The patient is a 28 year-old female seen in the office with left shoulder and right knee pain. She is under work up for Ehler danlos syndrome. She has been having issues for many years. She is in the office with an MRI of the knee and shoulder.
The MRI was reviewed and discussed; for her right knee pain it has no fracture, dislocation, marrow replacement process, or osteochondral lesion is identified.
The distal quadriceps tendon, patella, and patellar ligament appear within normal limits. 0.6 x 0.9 x 1.7 cm lobular oval lesion that is low signal on TI and heterogeneous signal on T2 is identified between the lateral patellar facet and anterior femur in the patellofemoral joint region and may represent fibrotic changes.
The anterior cruciate ligament, posterior cruciate ligament, medial collateral ligament, and lateral collateral ligament are intact. No soft tissue mass or abnormal signal in the musculature is identified. An oblique tear in the posterior horn of the medial meniscus is identified. The lateral meniscus is intact with no tear identified.
With impression of Oblique tear in the posterior horn of the medial meniscus. 0.6 x 0.9 x 1.7 cm lobular oval lesion that is low signal on TI and heterogeneous signal on T2 is identified between the lateral patellar facet and anterior femur in the patellofemoral joint region and may represent fibrotic changes.
For her left shoulder pain; the acromioclavicular joint is intact. There is rotator cuff peritendinitis and subacromial bursitis without evidence of rotator cuff tendon tear. The labral complex is intact.
The biceps tendon is normal. The glenohumeral joint is otherwise normal with impression of rotator cuff peritendinitis and subacromial bursitis without evidence of rotator cuff tendon tear and no other internal joint derangement.
MRI showed lesion in the lateral margin of the patella as well as medial meniscus tear. We discussed treatment options and opted for surgical management. We discussed the risks and benefits including infection, bleeding, injury to adjacent nerves and vessels, inability to heal, need for repeat surgery, need for rehabilitation amongst others.
We also discussed the possible need for biopsy and debridement of the lesion. We discussed systemic complications including blood clots, cardiac, pulmonary, and neurological complications including death. The patient understood and signed an informed consent.
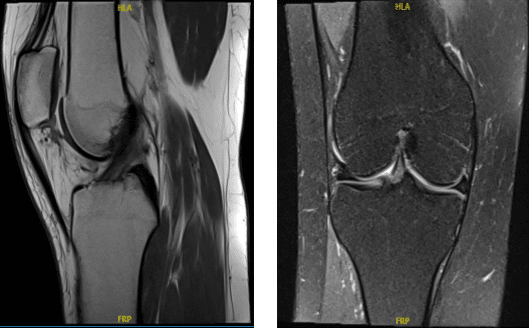
MRI Right knee non-contrast
The patient was taken to the operating room where she was placed on a well-padded operating room table. General anesthesia was induced. Right lower extremity was prepped and draped aseptically in the usual fashion. A tourniquet was applied. Time-out was called.
A lateral entry portal was made and an arthroscope was inserted. The Medical entry portal was then made with a spinal needle. Examination of the patellofemoral compartment showed fraying of the cartilage along the lateral border with possible fibrosis.
Examination of the medial compartment showed intact medial meniscus. A thorough examination of the medial meniscus was done but no tear could be found. There was grade 1 to grade 2 triple lesion of the cartilage of the medial femoral compartment which was debrided with the use of shaver.
Examination of the intercondylar notch showed intact ACL. Examination of the lateral compartment showed intact cartilage as well as meniscus. Examination of the patellofemoral compartment again showed intact patellar cartilage except for the central border and intact trochlear cartilage.
Debridement of the lateral margin of the patella was performed with the use of shaver followed by curettes. A biopsy was taken of the lateral margin of the patella and sent for examination. The final pictures were taken of the same.
The knee was thoroughly irrigated and drained. Closure was done with the use of #3-0 nylon. Dressing was done with the use of Xeroform, 4 x 8s, ABD, Ace wrap, and Webril. The patient was extubated and moved to recovery in a stable condition.
The patient seen in the office for her one week post operative visit, no x-rays were needed. She has swelling and pain. She is using a single crutch but denies fever, chills, she also has left shoulder pain and she is under work up for Ehler danlos syndrome. She has been having issues for years.
Biopsy was reported as normal tissue. After three weeks the patient went to the office for her follow up checkup, no x-rays were needed, she has no fever and chills and she has been working with PT and improving well.
After the operation, the patient recovered well and kept up with physical therapy. The patient returned for a follow-up visit and her knee had much improved.
Disclaimer – Patient’s name, age, sex, dates, events have been changed or modified to protect patient privacy

Dr. Vedant Vaksha
I am Vedant Vaksha, Fellowship trained Spine, Sports and Arthroscopic Surgeon at Complete Orthopedics. I take care of patients with ailments of the neck, back, shoulder, knee, elbow and ankle. I personally approve this content and have written most of it myself.
Please take a look at my profile page and don't hesitate to come in and talk.
