Case Study: Meniscal Repair Of The Medial Meniscus,
Partial Meniscectomy Of The Lateral Meniscus
And Microfracture Of The Right Knee
The patient, a 25-year-old female was involved in a motor vehicle accident a year ago. The patient also had an injury to the neck, lower back, and left shoulder which are getting better. The patient had pain on the inner side of the knee with a feeling of instability.
The pain in the right knee is severe to extremely severe in intensity. The patient describes the pain as sharp, dull, stabbing, throbbing, aching, burning. The pain is constant/ intermittent and does not disturb sleep.
The pain is associated with swelling, bruising, weakness, gait problem, giving way, and limping. The pain is not associated with tingling, numbness, radiating pain, bowel, or bladder abnormality.
The problem has been getting worse since it started. Walking, standing, lifting, exercise, twisting, bending, stairs, make the symptoms worse. Rest, ice, lying down makes the symptoms better. The patient is currently working as a paramedic and the pain is interfering with her day to day life.
The patient had previously tried conservative treatment in the form of physical therapy, heat therapy, and cortisone knee injections with minimal relief.
The patient does not smoke or uses recreational drugs. She has seasonal allergies. She had a right knee meniscal repair and TMJ surgery. Currently, she is on Vicodin, tizanidine, cyclobenzaprine, Protonix, and ASA (DVT prophylaxis).
On general physical examination, the patient was calm conscious cooperative, and well oriented to time place and person. The gait of the patient was steady but antalgic. Upon examination of the right knee, the patient is tender to palpation along the medial joint line and has an effusion.
She also has tenderness along the medial and lateral patellofemoral joint line. The patient has discomfort with McMurray’s maneuvers, and the knee is stable. They lack full flexion secondary to the effusion but have full extension. There 5/5 strength in bilateral lower extremities and the distal neurovascular is intact. There are no erythema, warmth, or skin lesions present.
On examination of the contralateral extremity, the patient is nontender to palpation and has an excellent range of motion, stability, and strength.
The MRI showed a medial meniscus tear on the periphery (ramp lesion). We discussed treatment options and the patient opted for surgical management. We discussed risks, benefits, and complications of surgical management including bleeding, infection, injury to adjacent nerve and vessels, need for repeat surgery, rehabilitation, need for wearing a knee immobilizer, and among others. The patient understood and signed informed consent.
PREOPERATIVE DIAGNOSIS: Medial meniscus tear
POSTOPERATIVE DIAGNOSES:
- Medial meniscus tear.
- Lateral meniscus tear.
OPERATION:
- Meniscal repair of the medial meniscus on the right knee.
- Partial meniscectomy of the lateral meniscus of the right knee.
- Microfracture of the right knee.
DESCRIPTION OF THE PROCEDURE: The patient was taken to the operating room, where he was placed on a well-padded operating room table. General anesthesia was induced. A tourniquet was applied to the mid-thigh of the right side. An examination under anesthesia was performed and the knee was found to be stable.
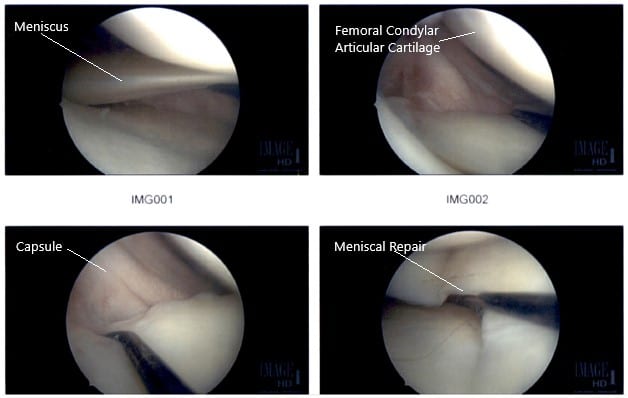
Intraoperative Arthroscopic Images of the right knee.
There was no ligament laxity. Preoperative antibiotics were given. The right lower extremity was prepped and draped in an aseptic condition. The tourniquet was inflated. A lateral entry portal was made and the arthroscope was introduced. The patellofemoral joint was examined and the medial compartment was examined and there was a near-complete tear of the posterior horn of the medial meniscus from the capsule.
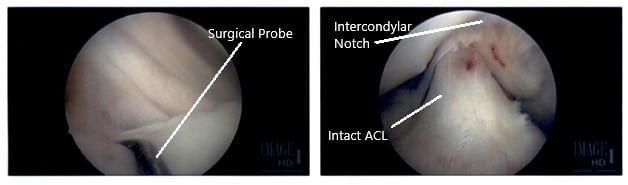
Intraoperative Arthroscopic Images of the right knee.
The decision to repair it was taken. The margins were probed using rasp and shaver. The meniscus was approximated onto the capsule and fixed using FasT-Fix Nephew curved x2. Good opposition was achieved. The sutures were cut after the notch. The all-inside technique was used. Final pictures were taken.
Finally, the scope was moved into the intercondylar area, where the ACL was found to be intact. The scope was moved to the lateral compartment, where there was faying of the posterior horn near the root of the lateral meniscus. It was debrided using shavers and punch. The scope was moved to the patellofemoral joint, which was found to be in good condition.
There was no arthritic patch over the cartilage. The scope was moved to the medial portal and the knee was re-examined again. The findings were confirmed and saved.
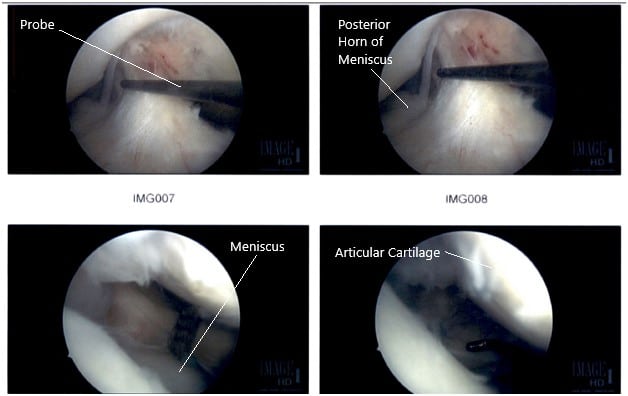
Intraoperative Arthroscopic Images of the right knee.
The lateral meniscal tear was further debrided and the final pictures were taken. At the end of the procedure, a micro punch was also used to put 4 to 5 holes into the intercondylar area. Fat globules and fresh blood could be seen coming out of those holes. The knee was irrigated copiously and closed using nylon #4-0. The dressing was done.
Postop protocol: The patient is advised to wear a Bledsoe brace and ambulate with it fixed in full extension only. She can unlock it and bend the knee up to 90 degrees when she is not weight-bearing. She can take up the dressing in about three days and have a shower. She will visit the office in a week and have the stitches will be removed. She can loosen the brace while sleeping or resting. She is to use crutches and bear weight as tolerated.
Disclaimer – Patient’s name, age, sex, dates, events have been changed or modified to protect patient privacy.

Dr. Suhirad Khokhar
My name is Dr. Suhirad Khokhar, and am an orthopaedic surgeon. I completed my MBBS (Bachelor of Medicine & Bachelor of Surgery) at Govt. Medical College, Patiala, India.
I specialize in musculoskeletal disorders and their management, and have personally approved of and written this content.
My profile page has all of my educational information, work experience, and all the pages on this site that I've contributed to.
