Case Study: Knee Arthroscopic Chondroplasty:
Medial and Lateral Meniscectomy with Cortisone Injection
in a 58 year-old patient
The goal of an arthroscopy is to look for discomfort or injury in the joint. It also results in a diagnostic that is excellent for treating the joint and is, in most circumstances, a long-term solution for the patient.
Not all knee discomfort is severe. But if left untreated, some knee illnesses and injuries, including osteoarthritis, can cause disability, joint damage, and excruciating pain. Additionally, even a slight knee injury increases the likelihood that you’ll suffer from additional problems in the future.
A 58-year-old patient was in our office with complaints regarding her bilateral knee pain and does not know how she sustained her injury or when the pain started. She was diagnosed with a tear on the meniscus right knee, and Baker had both knees.
She was treated with cortisone injections and gel shots but has no relief now. For aggravating factors, patients report standing, walking, weight bearing, exercise, upstairs, downstairs, and nighttime.
For associated symptoms, she reports weakness, swelling, catching/locking, popping/clicking, buckling, tender to the touch, and pain with motion but reports no numbness, no tingling, no redness, no warmth, no ecchymosis, no grinding, no instability, no radiation, no drainage, no fever, no chills, no weight loss, and no change in bowel/bladder habits.
For location, she reports bilateral. For quality, she reports stabbing, sharp, frequent, constant, and worsening. For severity, she reports severe.
She presented her Xray results, for her left knee there are mild osteoarthritic degenerative changes. For the right knee, there are moderate osteoarthritic degenerative changes. There are no fractures and there are no acute fractures.

Left knee X-ray
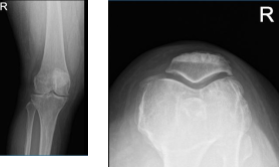
Right knee X-ray
The patient brought an MRI results, for her left knee, denudation of articular cartilage in the anterior compartment of the knee and tricomparmental marginal bony spurring. Intrasubstance degeneration in the posterior horn of the medial meniscus.
No definite surfacing medial or lateral meniscal tear is seen. Moderate sized Baker’s cyst. For the right knee, Complex degenerative tear in the medial meniscus extending from the body into the posterior horn into the posterior root with extrusion. Tricomparmental articular cartilage denudation with marginal bony spurring.
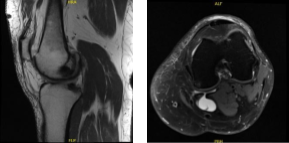
MRI-3T Left knee non-contrast
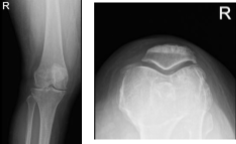
XR of Right Knee Lateral Oblique View
We discussed treatment options and the patient opted for surgical management. discussed risks and benefits including infection, bleeding, injury to adjacent nerves and vessels, nonhealing, need for repeat surgery, need for cortisone injections in future, knee stiffness and knee arthritis, need for knee replacement in the future, systemic complications, etc., cardiac, neurological, pulmonary complications and even death.
The patient understood and signed an informed consent.
The patient was taken to the operating room where she was placed on the well-padded operating table. Anesthesia was induced. Preoperative antibiotics were given. The tourniquet was applied on the right thigh. Cortisone injection was given in the left knee using 80 mg of Depo-Medrol and 7 cc of Naropin 0.5%.
The right lower extremity was prepped and draped aseptically in the usual fashion. Lateral entry portal was made, and an arthroscope was entered. Examination of the patellofemoral joint showed a grade 3 to grade 4 osteoarthritis with chondral flap.
Examination of the medial tibiofemoral compartment showed arthritis of the medial femoral condyle as well as tear of the medial meniscus in the posterior horn and the body. The Medical entry portal was made with the use of a spinal needle.
The shaver was used to debride the knee. With the use of upbiter and straight biter as well as shaver, the medial meniscectomy was performed to balance the margins. There was a degenerative tear of the root also. This was debrided. The posterior wound was still intact.
Examination of the infrapatellar notch showed degenerative ACL and intact. There was synovitis, which was debrided. Examination of the lateral tibiofemoral compartment showed arthritis of the lateral femoral condyle as well as tear of the lateral meniscal medial margin.
Debridement was done with the use of biters as well as shavers. There was also an examination of the medial tibiofemoral compartment. There was grade 3 to grade 4 osteochondral damage of the medial femoral condyle. This was debrided using shaver.
The scope was entered into the patellofemoral joint where there was grade 3 to grade 4 osteoarthritis of the patella as well as trochlea which was debrided using the shaver. There was chondral flap, which was excised with biters and shavers.
The arthroscope was entered from the medial portal and further balancing of the medial and lateral meniscus was performed and the findings were re-examined and confirmed. The knee was thoroughly irrigated, and final pictures were taken and saved. The knee was drained and closed using #3-0 nylon.
Then, 9 cc of Naropin 0.5% mixed with 40 mg of Depo-Medrol was injected into the knee. The dressing was done using Adaptic, 4 x 4s, Webril, Ace wrap. The tourniquet was removed. The patient was extubated and moved to recovery in a stable condition.
We have decided to proceed with formal physical therapy as well as a home exercise program for rehabilitation of the knee. The patient did well after the surgery and continued physical therapy. The patient checked in for a follow up visit after a month and saw significant improvement in her knee.
Disclaimer – Patient’s name, age, sex, dates, events have been changed or modified to protect patient privacy.

Dr. Vedant Vaksha
I am Vedant Vaksha, Fellowship trained Spine, Sports and Arthroscopic Surgeon at Complete Orthopedics. I take care of patients with ailments of the neck, back, shoulder, knee, elbow and ankle. I personally approve this content and have written most of it myself.
Please take a look at my profile page and don't hesitate to come in and talk.
