Case Study: Knee Surgery: Medial Meniscus
in a 68 year-old female
A lateral meniscus tear affects the semicircular cartilage that lines the exterior of the knee joint. Through twisting or a traumatic injury, the McMurray test is one of the primary examinations for meniscus injuries. Your knee will be flexed by your doctor before being straightened and rotated.
A meniscus tear is put under stress by this. If you have a meniscus tear, this movement may hurt, click, or make the joint seem clunky. stiffness or swell. Pain, particularly when you rotate or twist your knee. Having trouble fully straightening your knee. attempting to move your knee and feeling as though it is immobile.
A 68 year-old female patient was seen in the office with right knee pain at Mather hospital and put in a knee brace and referred to us. MRI were reviewed and discussed by the doctor; Complex tear of the medial meniscus.
Mild MCL sprain superimposed on chronic scarring. Moderate chondromalacia patella and mild cartilage loss in the medial compartment. Moderate joint effusion.
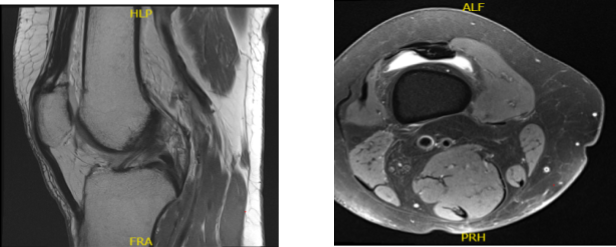
MRI Right Knee Non-contrast
After two days the patient came back to the office and we discussed the treatment options for the patient’s diagnosis, which included: living with the extremity as it is, organized exercises, medicines, injections and surgical options. We also discussed the nature and purpose of the treatment options along with the expected risks and benefits.
The patient has expressed a desire to proceed with surgery, and We think that is a reasonable option.
We educated the patient regarding the inherent and unavoidable risks which include, but are not limited to: infection, stiffness, damage to nerves and blood vessels, blood loss possibly requiring transfusion, blood clots, persistent or worsening pain, loosening or failure of implants, instability, tingling or numbness, anesthesia and systemic complications including cardiac, pulmonary, neurological complications and even death were discussed at length.
We also talked about the possibility of not being able to return to prior activities or employment, the need for future surgery, and complex regional pain syndrome.
We discussed treatment options and the patient opted for surgical management. We discussed risks and benefits including infection, bleeding, injury to adjacent nerves and vessels, rehabilitation, knee stiffness, need for knee replacement in future, systemic complications including blood clot, cardiac, pulmonary, neurological complications including death. The patient understood and signed an informed consent.
The patient was taken to the operating room where she was placed on a well-padded operating room table. General anesthesia was induced. Right lower extremity was prepped and draped aseptically in the usual fashion after application of low thigh tourniquet. Time-out was called.
Preoperative antibiotic was given. Tourniquet was elevated. Lateral entry portal was made through a lateral parapatellar incision. Arthroscope was inserted. A medial parapatellar incision was given after guiding it with a spinal needle.
Examination of the medial tibiofemoral compartment showed a complex tear of the posterior horn of the medial meniscus along with grade 2 to grade 3 osteoarthritis of the medial femoral condyle.
Debridement of the meniscus was done with use of shaver and biters. Debridement chondroplasty was also performed with the use of a shaver. Examination of the intercondylar notch showed intact ACL. Examination of the lateral tibiofemoral compartment showed intact meniscus and cartilage.
Examination of the patellofemoral compartment showed grade 3 to grade 4 osteochondral lesion of the lateral facet of patella. Trochlea was intact. Debridement of the patella was done with the use of a shaver.
Arthroscope was inserted through the medial portal and shaver was inserted to the lateral portal and further balancing of the medial meniscus as well as chondroplasty of the patella was performed. Final pictures were taken and saved. Knee was thoroughly irrigated and drained.
Closure was done with the use of # 3-0 nylon. Dressing was done with 20 cc of 0.5% Marcaine mixed with 40 mg of Depo-Medrol was injected into the knee. Dressing was done with the use of Xeroform, 4 x 8, ABD, Webril, Ace wrap. The patient recovered. The patient was extubated and moved to recovery in stable condition.
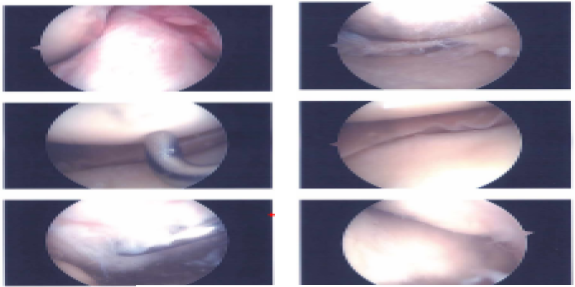
Intraoperative images
She is here today for her one-week post-operative visit, no X-rays were needed. Pain is well controlled. Denies fever, chills. After the doctor discussed the treatment options we have decided to proceed with formal physical therapy as well as a home exercise program for rehabilitation of the knee.
We went over the arthroscopic pictures and removed the stitches during today’s visit. We will continue with ice and elevation of the knee to decrease swelling and pain. We will continue to utilize early mobilization and mechanical prophylaxis to reduce the chances of a deep vein thrombosis.
We will wean them off any narcotic medications and progress to anti-inflammatories and Tylenol as long as there are no contraindications to these medications.
We also discussed the risk and benefits and common side effects of taking these medications at today’s visit. I will see them back in three weeks’ time to evaluate their progress. They will call us in the interim if they have any questions or concerns prior to their follow up visit.
The doctor discussed treatment options including PT, MRI, Injection, surgery, and we agreed to go with conservative management for now. PT to be started as discussed. After discussing the options for treatment and the risks of injection, the patient wished to proceed with the injection to reduce pain and swelling.
After a sterile prep, 7cc of 1% Lidocaine and 80mg of depo-medrol were injected into the right knee. The patient tolerated the procedure well and there were no complications. Post injection pain, blood sugar elevation, skin discoloration, fatty atrophy and the signs of infection were discussed in detail.
After a couple of times the patient was seen in the office we agreed to go with conservative management and physical therapy. The patient has a regular checkup every four weeks to evaluate progress.
Disclaimer – Patient’s name, age, sex, dates, events have been changed or modified to protect patient privacy.

Dr. Vedant Vaksha
I am Vedant Vaksha, Fellowship trained Spine, Sports and Arthroscopic Surgeon at Complete Orthopedics. I take care of patients with ailments of the neck, back, shoulder, knee, elbow and ankle. I personally approve this content and have written most of it myself.
Please take a look at my profile page and don't hesitate to come in and talk.
