Case Study: Left Hip Total Replacement
in a 54-year-old female with Hip Arthritis
A 54-year-old female was referred to our office by her primary care physician with complaints of bilateral hip pain (left greater than right) and difficulty walking. The patient stated she sustained a work-related injury to her left hip 2 years ago. She feels the pain has since progressed and affected her right hip.
The patient is employed as a UPS driver but currently not working. Her work required her jumping in and out of the truck, high paced walking, squatting and lifting heavyweight. She states she has been unable to carry on her work duties for the past 4 months secondary to pain. She was finding it increasingly difficult to perform her daily activities at home. She used a cane as a walking aid.
The patient described the onset of pain as insidious located anteriorly in the left groin. The intensity of the pain was described as moderate (5/10) which was a dull ache in character. Activities such as walking fast or climbing stairs exacerbated the pain. She additionally complained of stiffness in the left hip after sitting for prolonged periods of time. She denied any radiation of the pain.
The patient stated that the frequency of hip pain was increasing resulting in disturbed sleep. She was stressed by the fact she was unable to perform her daily activities and was unable to return to work. She had tried conservative management in the form of physical therapy, heat pads, use of a cane and hip injections but without any significant relief.
The patient was a nonsmoker, nondrinker, and no significant past medical history. Her current medications included over the counter vitamins and supplements. She denied any history of steroid intake, multiple joint pain, lower back pain, and neck stiffness, epilepsy, significant trauma. Her family history was positive for Osteoarthritis of the bilateral knee in her mother. She had no known drug allergies.
On her office visit, she was calm, conscious, cooperative and well oriented to time, place and person. She was ambulatory with a bipedal, stable, coordinated and antalgic gait (decreased stance phase on the left side).
On her physical examination, there was no leg length discrepancy. Both the anterior superior iliac spines were at the same level with no exaggerated lumbar lordosis. There was no scar, sinuses or swelling in the Scarpa’s triangle. There was no lymphadenopathy or any mass/induration.
Muscle bulk was normal and strength was full in bilateral lower extremities. There was no thickening or broadening of the bilateral trochanters. The range of motion of the left hip was full with painful internal and external rotation. The right hip and bilateral knee and ankles were normal. There was no distal neurological deficit and both limbs had palpable 2+ dorsalis pedis and posterior tibial artery.
Her imaging studies revealed arthritis changes in both her hips. Considering her lifestyle limiting hip pain, she was advised to undergo bilateral hip total replacement. Risks, benefits, and alternatives were discussed with her as well with her husband at length. She agreed to go ahead with left hip replacement.
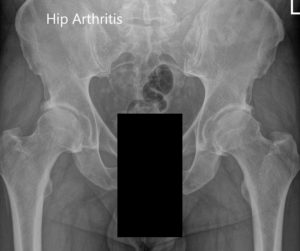

Preoperative X-ray of the pelvis AP view and the lateral view of the left hip.
Operation: Left total hip arthroplasty using a posterolateral approach.
Implant used: Titanium hemispherical shell 60 mm with a 6.5 cancellous screw, 6.5 mm in diameter, 35 mm in length with ceramic femoral head 36 mm, 0-degree polyethylene with 127-degree neck angle hip stem size 5.
Description of the procedure: The patient was brought to the operating room after obtaining informed consent and signing the correct surgical site. The risks, benefits, and alternatives were extensively discussed with the patient prior to the procedure. The patient was brought to the operating room and anesthesia was obtained by the anesthesiologist.
The patient was definitively positioned with the left hip up and the left hip was then draped and prepped in the usual sterile manner. The straight incision centered over the greater trochanter was used for the arthrotomy.
Skin and subcutaneous tissues were then incised. The fascia was then divided. The robotic arm images were used for the planning of the surgery.
The acetabulum was then exposed. The remainder of the labrum was then debrided. The acetabulum was reamed and the final shell was then placed into position in the correct abduction and anteversion.
The shell was then placed over the cup after the placement of the screw. Attention was then turned towards the femur. The remainder of the tissue on the undersurface of the greater trochanter was then removed. The femur was then sequentially broached and the final broach was left into position.
The trunnion was then placed over the shell and the head was then placed over the trunnion. The pre-robotic plan was used in the assessment of the height. The lesser trochanter to center distance was also measured preoperatively before making the neck resection and was also compared after placement of the trial component. The hip was then reduced and trialed through a full range of motion and the hip was stable in all physiological range of motion.
The hip was dislocated. Trial components were then removed. The final components were then placed into position. The hip was then reduced again. A thorough lavage was given. The posterior soft tissue structures were then tacked to the greater trochanter through transosseous tunnels. Thorough lavage was given.
The fascia was closed, cutaneous tissues were closed, subcutaneous tissues were closed. The skin was closed using staples. Sterile dressing was then applied over the wound and the patient was then transferred to the postoperative care unit in stable condition.

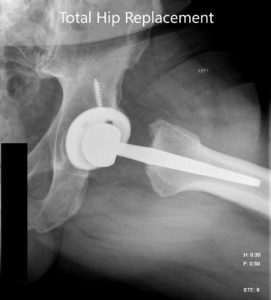
Postoperative X-ray images showing AP view and frog legged lateral view.
The patient had an unremarkable recovery postoperatively. Her staples were removed from the left hip surgical incision. The incision was intact with no signs or symptoms of infection. The patient was educated about hip precautions to prevent dislocation. She was advised for physical therapy.
The physical therapy was directed for gait training, home safety and fall prevention, and muscle strengthening. She was advised to walk as tolerated. She was prescribed aspirin 325mg BID for deep vein thrombosis prophylaxis.
After 3 months, she was walking without pain. She was advised to discontinue aspirin and continue the home exercise program with gradual weaning of hip precautions. She was happily back driving her car and performing her daily activities, and returned to light duty at work. She was happy to be off using the cane and reported that her gait has improved significantly. She reportedly experienced less pain in the right hip. She follows up as needed.

Dr. Suhirad Khokhar
My name is Dr. Suhirad Khokhar, and am an orthopaedic surgeon. I completed my MBBS (Bachelor of Medicine & Bachelor of Surgery) at Govt. Medical College, Patiala, India.
I specialize in musculoskeletal disorders and their management, and have personally approved of and written this content.
My profile page has all of my educational information, work experience, and all the pages on this site that I've contributed to.
