Case Study: Management of 55-year-old Female with Left Knee
Quadriceps Tear, Lateral Meniscus Tear, and Partial ACL Tear
The patient is in our office, with complaints of left knee pain and loss of function for the past 1 month. The patient sustained an injury in a fall, the patient states she can not put pressure on the knee. The patient also states she feels a gap between the knee cap. The patient works as a security guard at a clinic and sustained the injury when she was trying to restrain a patient and fell.
The pain is extremely severe in intensity (10/10). The pain is constant. The problem has been getting unchanged since it started. Ice and ibuprofen make the symptoms better. She is currently taking muscle relaxants and NSAIDs for pain. She is unable to walk unassisted and uses a cane for walking.
The patient has a medical history significant for diabetes and psoriasis both well controlled with medications. She denied any past surgical history. The patient is allergic to shellfish. She is a non-smoker and consumes alcohol socially.
On physical examination, the patient was calm conscious cooperative, and well oriented to time place and person. On examination of the left knee, there was moderate swelling. The patient was unable to do active straight leg raise. A void was felt over the proximal pole of the patella. The range of motion was restricted secondary to pain. There was no distal neurovascular deficit.
The examination of the contralateral knee was unremarkable.
X-ray of the left knee suggested a soft tissue swelling anterior to the patella and patellar tilt.
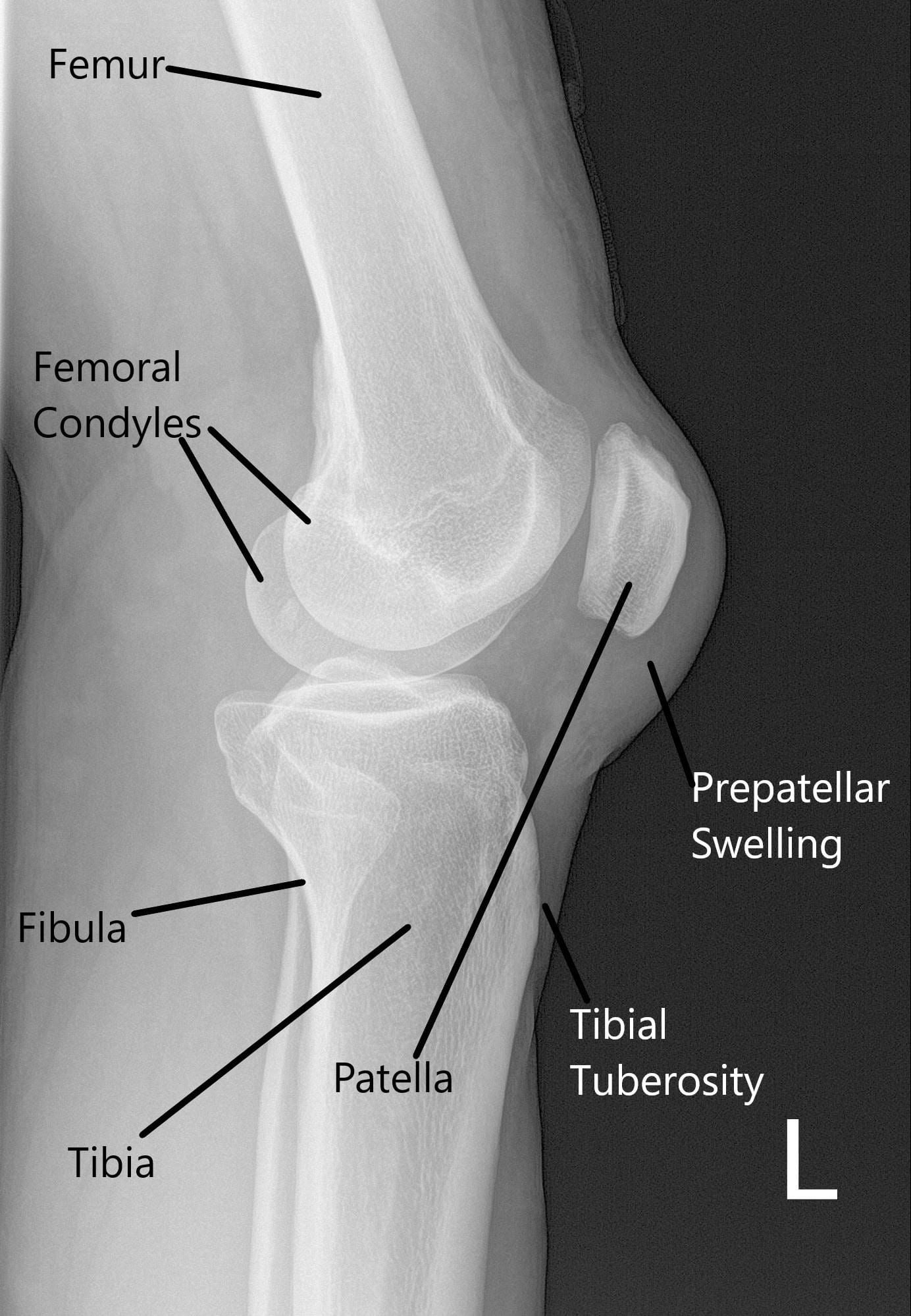
X-ray of the left knee in lateral view.
MRI suggested a complete rupture of the quadriceps tendon at the patellar attachment. The joint effusion communicates through the tendon defect with a prepatellar fluid collection. Low-grade intrasubstance tear at the origin of the ACL. Radial tear at the free edge of the lateral meniscal body.
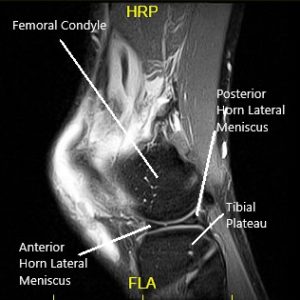
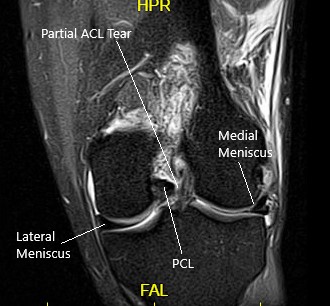
MRI of the left knee in the sagittal and coronal view.
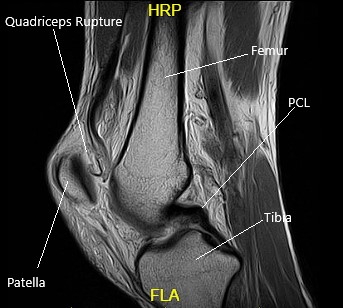
MRI of the Left Knee in the sagittal section.
All treatment options including surgical and nonsurgical were discussed with the patient at length. Risks, benefits, and alternatives were also discussed with the patient. The patient agreed to go ahead with the surgical procedure.
PREOPERATIVE DIAGNOSES:
- Left knee quadriceps tear.
- Left knee lateral meniscus tear.
- Left knee partial tear of the ACL.
POSTOPERATIVE DIAGNOSES:
- Left knee quadriceps tear.
- Left knee lateral meniscus tear.
- Left knee partial tear of the ACL.
- Grade 2 to grade 3 chondral damage trochlea.
OPERATION:
- Knee arthroscopy with partial lateral meniscectomy.
- Arthroscopic chondroplasty of Patella.
- ACL debridement, left knee.
- Open repair of the quadriceps, left knee.
PROCEDURE: The patient was taken to the operating room where he was put on a well-padded operating table. General anesthesia was induced. The left lower extremity was put in a high tourniquet. The left knee was prepared aseptically and draped in the usual fashion. A time-out was called. A tourniquet was applied and inflated. Tourniquet time was 103 minutes.
A left lateral entry portal was made and the scope was entered. The knee was lavaged with a lot of fluid to clean up the blood. The visualization was not properly to the blood.
The scope was moved to the medial tibiofemoral compartment. The medial meniscus was intact. There was no chondral damage. The scope was moved to the intercondylar area where partial ACL tear of the lateral side was found. The debridement was done. The rest of the 90% of ACL was intact.
The scope was moved to the lateral tibiofemoral compartment where the tear of the medial edge of the lateral meniscus was present. The tear was cleaned using right-sided biters and shavers. The rest of the lateral meniscus was intact. There was no chondral damage.
The scope was moved to the patellofemoral joint where trochlea grade 2 to grade 3 chondral damage was found. The chondral damage was debrided from the medial portal and followed by the lateral portal. Copious lavage was performed. Arthroscopic pictures were taken and saved.
The scope was removed. The knee was extended. The table was extended and a proper draping was performed. A midline vertical incision was put and centered over the superior pole of the patella.
The quadriceps tendon was found to be completely ruptured. The tendon was debrided. The stump of the tendon was over the patella was removed. The bone was decorticated to fresh bleeding margins. Three transosseous tunnels were made and silk ties were put for future use.
Now, the tendon was sutured using #5 FiberWire with a Krackow stitch x2. The four tails of the #5 FiberWire were passed through the three tunnels into the patella. The lateral and medial FiberWires were tied on to each other and the knots were buried.
The lateral and the medial retinaculum was repaired using #2 FiberWire. After proper closure, the wound was again lavaged. The closure of the skin was performed using Vicryl #2-0 and Monocryl #4-0.
The arthroscopic portals were closed using nylon #4-0. The dressing was performed using Steri-Strips, Adaptic, 4 x 4s, ABD, Webril, and Ace wrap. The tourniquet was removed. The patient was extubated and moved to the recovery unit in a stable condition.
Disclaimer – Patient’s name, age, sex, dates, events have been changed or modified to protect patient privacy.

Dr. Suhirad Khokhar
My name is Dr. Suhirad Khokhar, and am an orthopaedic surgeon. I completed my MBBS (Bachelor of Medicine & Bachelor of Surgery) at Govt. Medical College, Patiala, India.
I specialize in musculoskeletal disorders and their management, and have personally approved of and written this content.
My profile page has all of my educational information, work experience, and all the pages on this site that I've contributed to.
