Case Study: Knee Arthroscopy: Medial and Lateral
Meniscectomy with Microfracture in a 63 year-old female
Microfracture is a surgical method that was created to repair chondral defects, which are damaged areas of articular cartilage in the knee, whereas meniscectomy is a crescent-shaped ring of thick, rubbery cartilage linked to the shinbone or tibia.
A 63 year-old female patient visits the office with right knee pain. Patient states that a few days ago, she was exercising and started feeling pain in right knee suddenly. She has no past medical history and is not taking any medications. NKDA.
She is active with gym and exercises which she is not able to do because the pain is worsened every time she is doing it. She felt her limp hurt and also had swelling along with popping. Upon examination, considering the difficulty in daily activities as well as recreation including gym and exercises, we agreed to go with 3 tesla MRI of the right knee.
MRI were reviewed and discussed by the doctor, The anterior cruciate, posterior cruciate, medial collateral, and lateral collateral ligaments are intact. A horizontal tear is present at the junction of the body and posterior horn medial meniscus with a 4 mm fragment flipped into the medial joint recess.
A small horizontal tear is present at the junction of the body and anterior horn lateral meniscus. The quadriceps and patellar tendons are intact. The medial and lateral patellofemoral ligaments are unremarkable. A small amount of knee joint fluid is present.
Superficial cartilage irregularity is present in all 3 compartments with almost full-thickness cartilage loss in the medial aspect of the patella that is associated with subchondral bone marrow edema.
Overall, the bone marrow signal is age-appropriate. There is also a small popliteal cyst. The popliteus muscle and tendon are intact and the iliotibial band is within the normal limits and the posterior lateral corner is unremarkable.
Horizontal tear the junction of the body and posterior horn medial meniscus with fragments flipped into the medial joint recess. Horizontal tear at the junction of the body and anterior horn lateral meniscus. It has tricompartmental degenerative changes with cartilage loss most pronounced in the medial aspect of the patella and popliteal cyst.
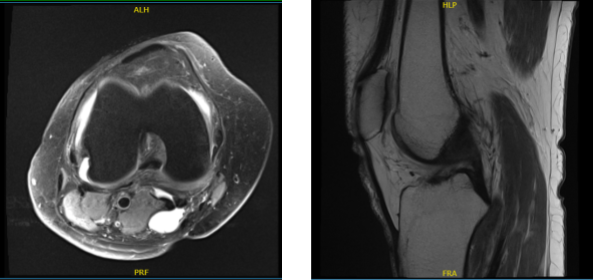
MRI of knee non-contrast
We discussed the treatment options for the patient’s diagnosis, which included: living with the extremity as it is, organized exercises, medicines, injections and surgical options. We also discussed the nature and purpose of the treatment options along with the expected risks and benefits.
We also explained that there is no guarantee that all the function and strength will return. We have discussed the surgical procedure as well as the realistic expectations regarding the risks, outcome and post operative protocol.
The patient has understood and expressed a desire to proceed with surgery and signed an informed consent.
The patient was taken to the operating room where she was placed on a well-padded operating table. General anesthesia was induced. Right lower extremity was prepped and draped aseptically in the usual fashion.
Preop antibiotic was given. Tourniquet was inflated. Time-out was called. Lateral anterior portal was made for the arthroscope and the examination of the knee was done. It showed osteoarthritic lesions on the posterior surface of the patella.
Examination of the medial compartment showed medial meniscus tear. The Medical entry portal was made using a spinal needle. Medial meniscectomy was performed using a shaver and biters.
Examination of the intercondylar notch showed intact ACL. Examination of the lateral tibiofemoral compartment showed a tear of the lateral meniscus, which was cleaned using biters as well as shaver.
Examination of the patellofemoral compartment showed osteoarthritic changes of grade 3 to grade 4. Decision for microfracture was done and was done to microfracture the posterior surface of the patella.
The scope was entered from the medial entry portal and findings reconfirmed and final balancing of the meniscectomy was performed. The knee was drained completely and irrigated and final pictures were saved.
Closure was done using # 4-0 nylon. Then, 40 mg of Depo-Medrol mixed with 9 cc of 0.5% Naropin was Injected Into the knee. Dressing was done using Adaptic, 4 x4, Webril and Ace wrap. The patient was extubated and moved to the recovery room in stable condition.
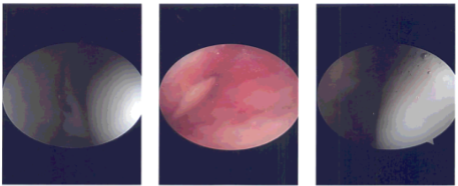
Intraoperative photo
After a week, the patient status post right knee arthroscopic lateral and med meniscectomy, patellar chondroplasty done. She is doing well, she has denied fever, chills and ambulating FWB without aid.
We have decided to proceed with formal physical therapy as well as a home exercise program for rehabilitation of the knee. We went over the arthroscopic pictures and removed the stitches. We advised the patient to continue with ice and elevation of the knee to decrease swelling and pain.
We also continue to utilize early mobilization and mechanical prophylaxis to reduce the chances of a deep vein thrombosis. We will wean them off any narcotic medications and progress to anti-inflammatories and Tylenol as long as there are no contraindications to these medications.
We also discussed the risk and benefits and common side effects of taking these medications. And the patient will be back every four weeks to evaluate their progress.
Disclaimer – Patient’s name, age, sex, dates, events have been changed or modified to protect patient privacy.
I am Vedant Vaksha, Fellowship trained Spine, Sports and Arthroscopic Surgeon at Complete Orthopedics. I take care of patients with ailments of the neck, back, shoulder, knee, elbow and ankle. I personally approve this content and have written most of it myself.
Please take a look at my profile page and don't hesitate to come in and talk.

