Case Study: Management of Three-Part
Fracture of the Left Proximal Humerus
The patient is a 54-year-old female presenting with complaints of left shoulder pain, swelling, and loss of function. The patient had a slip and fall in the bathroom yesterday afternoon. She noticed immediate swelling and pain. The patient did icing and took Advil for pain.
The patient is a school teacher, with a medical history significant for osteoarthritis, osteoporosis, and hypothyroidism. The patient’s current medications include bisphosphonates, calcium, vitamin D, and levothyroxine. The patient is a nonsmoker and denies the use of any illicit medications. The patient is allergic to shellfish.
On physical examination of the left upper extremity, there was swelling and warmth present over the left shoulder. There was tenderness to palpation over the greater tuberosity and the glenohumeral region. Upon movement of the shaft humerus, there was no movement of the humeral head. The distal neurovascular examination of the left upper extremity was normal.
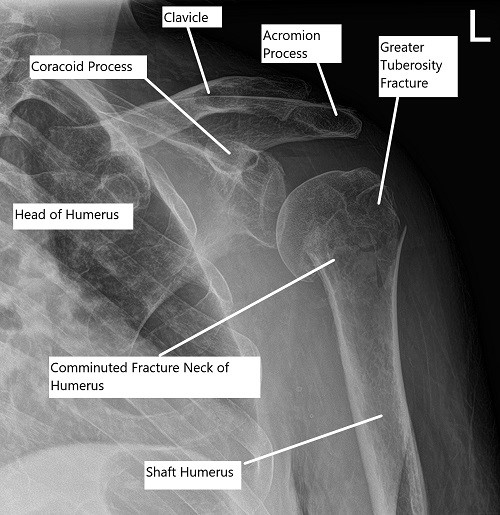
Pre-operative x-ray of the shoulder showing a three-part fracture of the proximal humerus.
Radiological studies in the form of an x-ray revealed a comminuted fracture of the humeral head and neck. A CT scan of the left shoulder revealed a comminuted proximal humeral fracture which is impacted and a slightly angulated fracture component at the surgical neck, a slightly displaced fracture fragment at the greater tuberosity, and a subtle nondisplaced fracture at the lesser tuberosity.
Various treatment options were discussed with the patient at length and the patient opted for surgical management. The risks, benefits, and potential complications were all discussed at length to the patient’s satisfaction. The patient verbalized agreement and signed the informed consent.
PREOPERATIVE DIAGNOSIS: Three-part displaced fracture of the left proximal humerus.
POSTOPERATIVE DIAGNOSIS: Three-part displaced fracture of the left proximal humerus.
OPERATION: Open reduction and internal fixation of the left proximal humerus using proximal humerus plate and combination of locking and non-locking screws.
DESCRIPTION OF PROCEDURE: The patient was taken to the operating room where he was placed on a well-padded operating table. General anesthesia was induced. The patient was put in a semi-reclining position. C-arm was brought in to see that the x-ray was visible in different views.
The patient was positioned appropriately and all bony prominences were well padded. Time-out was called. The preop antibiotic was given. The patient’s left upper extremity was prepped and draped aseptically in the usual fashion.
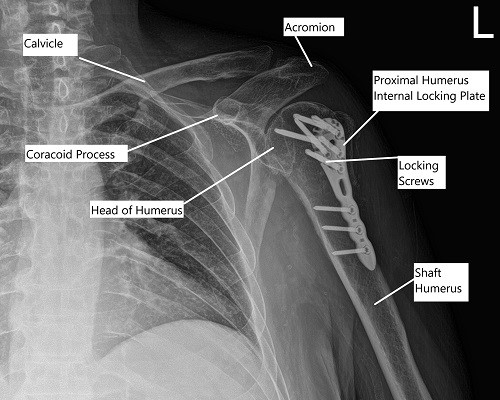
Post-operative x-ray of the left shoulder in AP view.
A lateral incision was made from the mid acromion distally along the shaft of the humerus. With sharp and blunt dissection, the fascia was removed. The acromion tip was reached and stay suture was put with 3-0 nylon at 4 cm from the acromial tip to restrict the dissection of the deltoid. The deltoid fibers were split in line with the incision and the incision and the proximal humerus was reached. Subacromial bursa was reached and excised.
The fracture was seen and cleaned. The fracture was reduced. A proximal humeral plate was chosen and inserted subperiosteally. The axillary nerve could be palpated along the medial aspect of the deltoid. The axillary nerve was elevated and the plate was passed underneath it.
A separate incision was made for reaching the distal fragment of the plate. With sharp and blunt dissection, the plate was reached and held with the sleeves. Finding the plate in an acceptable position, a K-wire was used to hold the plate in position. Fixation of the distal fragment was done with the use of one nonlocking screw and followed by fixation of the proximal fragment in a reduced position using multiple locking screws.
The fragment of the greater trochanter was also reduced with #0 FiberWire and sutured to the plate. Distal fixation was done with the use of three cortical screws. Final pictures were taken and saved in multiple positions and found to be acceptable. The wound was thoroughly cleaned and closed in layers using #0 Vicryl, #2-0 Vicryl, and Monocryl. The dressing was done using Dermabond, 4 x 4s, ABD, and Tegaderm. The patient was extubated and moved to recovery in a stable condition.
Disclaimer – Patient’s name, age, sex, dates, events have been changed or modified to protect patient privacy.

Dr. Suhirad Khokhar
My name is Dr. Suhirad Khokhar, and am an orthopaedic surgeon. I completed my MBBS (Bachelor of Medicine & Bachelor of Surgery) at Govt. Medical College, Patiala, India.
I specialize in musculoskeletal disorders and their management, and have personally approved of and written this content.
My profile page has all of my educational information, work experience, and all the pages on this site that I've contributed to.
