When the articular cartilage wears down to the point that the underlying bone is visible, an abrasion chondroplasty is done. A rotary burr is utilized in this treatment to scrape the bone tissue from the joint’s surface.
An orthopedic knee expert collects cartilage cells from the patient’s knee in order to execute a MACI operation. The surgeon transfers the cartilage cells that were collected to a lab, where the cells develop into new cartilage. The surgeon inserts the new cartilage into the knee’s injured area after it has recovered.
A 47 year-old patient presents with left knee pain that began one week ago. She works as a hemodialysis nurse at SBU and is out of work due to this pain. She is having pain, swelling, buckling and the swelling has decreased. She tried conservative management but had no benefit. The doctor advised her to do an MRI.
MRI was performed, reviewed and discussed by the doctor; the findings stated the Collateral Ligaments: The medial collateral ligament is intact. The lateral collateral ligament, biceps femoris tendon, iliotibial band, and popliteus tendon is intact.
Cruciate Ligaments: The anterior and posterior cruciate ligaments are intact. Menisci: The medial meniscus is intact. The lateral meniscus is intact. The Cartilage: There is a 9 x 6 mm full-thickness chondral defect in the midportion of the medial femoral condyle.
The chondral surfaces in the lateral compartment are intact. There is a focal area of chondral fissuring and partial-thickness cartilage loss in the central trochlea. Bones: The visualized osseous structures demonstrate normal bone marrow and cortical signal intensity without evidence of fracture, trabecular bone injury or dislocation.
No osseous lesions are identified. The Extensor Mechanism: The quadriceps and patellar tendons are normal. Joint: Large knee joint effusion. The soft tissues are otherwise normal. The neurovascular structures demonstrate normal course.
It has an impression of 9 x 6 mm full-thickness chondral defect in the midportion of the medial femoral condyle. Focal area of Chondral fissuring and partial-thickness cartilage loss in the central trochlea. Intact medial and lateral meniscus.
After discussing the options for treatment and the risks of injection, the patient wished to proceed with the injection to reduce pain and swelling. After a sterile prep, 7cc of 0.5% Marcaine and 80mg of depo-Medrol were injected into the left knee.
The patient tolerated the procedure well and there were no complications. Post injection pain, blood sugar elevation, skin discoloration, fatty atrophy and the signs of infection were discussed in detail.
MRI showed a focal osteochondral defect of the left femoral condyle. The rest of the knee looked good. We discussed treatment options and the patient opted for surgical management.
The patient was leaning towards possible repair and reconstruction of the osteochondral defects in an attempt to make it somewhat longer and avoid knee arthritis and early knee replacement. We discussed chondroplasty vs. osteochondral bone grafting vs. joint replacement surgery in the possible future.
The patient understood and agreed for arthroscopic chondroplasty and measurements. We discussed the risks and benefits including infection, bleeding, injury to the nerves and vessels, possible numbness, need for repeat surgery in case we need to do a repair or reconstruction, arthritis, rehabilitation, need in the surgery in the future, among others.
We also discussed the complications including blood clot, femoral artery complications or death. The patient understood and signed the informed consent.
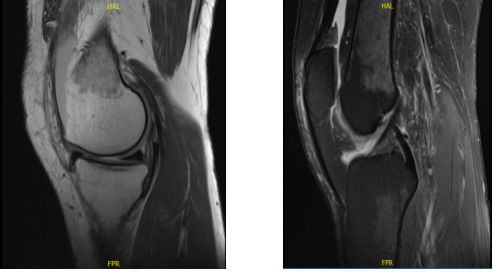
MRI-3T Left knee non-contrast
The patient was taken to the operating room and she was placed on the right sided operating room table. The patient was sedated and a time out was called. 10 cc of 2% Lidocaine mixed with .5% Marcaine without epinephrine was injected into the mid portal.
A total injection of 30 cc was injected into the left knee. Sedation was given to the patient. The left knee was prepped and draped aseptically in the usual sterile fashion. Compression was applied. The knee was put in a clamp. A timeout was called. Preoperative consent was given already.
The tourniquet was elevated to 250 mmHg. After exsanguination an incision was made. The lateral portal anesthesia was given. A medial anterior portal incision was made with the use of a spinal needle. There was arthritis along the medial femoral condyle and medial tibial plateau. The meniscus was intact.
There was a Grade IV defect of the medial femoral condyle which was debrided with the use of curette and debrided and abrasion chondroplasty was performed with the use of a curette. The defect was measured and was 1.5 cm by 1.5 cm.
Examination revealed an intact ACL. Examination noted lateral tibial tendon patellofemoral compartment showed intact cartilage. Examination of the patellofemoral compartment showed intact cartilage over the patella but there was Grade III to Grade IV osteochondral lesion of the trochlea.
Debridement of this lesion was performed to stable margins. The defect was measured to be 1.5 cm x 1 cm. All of the measurements were taken. All of the pictures were taken and saved. The knee was drained. Closure was done with 3-0 nylon.
Dressing was done with the use of Xeroform, double 4 x 8, Ace wrap, the tourniquet was deflated. The patient was extubated and brought to the recovery room in stable condition.
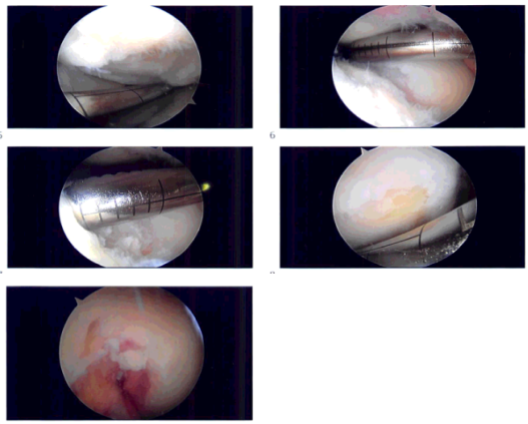
Intraoperative images
The patient seen in the office for her postoperative visit, no x-rays were needed. The patient is doing well, she denies fever and chills. After discussing treatment options, we have decided to proceed with formal physical therapy as well as a home exercise program for rehabilitation of the knee.
We went over the arthroscopic pictures and removed the stitches during the visits. We will continue with ice and elevation of the knee to decrease swelling and pain. We will continue to utilize early mobilization and mechanical prophylaxis to reduce the chances of a deep vein thrombosis.
We will wean them off any narcotic medications and progress to anti-inflammatories and Tylenol as long as there are no contraindications to these medications. We also discussed the risk and benefits and common side effects of taking these medications. The patient agreed for a MACI procedure in future.
After a month the patient went to the office for her follow up checkup, no x-rays were needed. The patient is doing well, she denies fever, chills. She is not able to straighten her knee and bend completely. She is working now with her Physical Therapy.
After 2 months the patient is here for her monthly checkup, upon the follow up consultations the patient is doing well, she has no fever, chills and she is now able to straighten her knee and bend completely. She has no restriction of movement and no pain. She is scheduled for MACI.
The patient was taken to the operating room for MACI procedures, she was placed on a well-padded operating table. General anesthesia was induced in the form of LMA.
Left lower extremity was prepped and draped aseptically in a usual fashion with a bump under the head and a lateral post. A time-out was called. Preop antibiotic was given. Tourniquet was not inflated for the procedure.
Incision was planned along the midline anterior to the patella. It was extended from the distal quadriceps to the tibial tuberosity. Deep dissection and flap were raised above the patellar retinaculum as well as the patella.
A medial parapatellar arthrotomy was done with the use of a sharp blade taking precautions not to injure the cartilage as well as the meniscus. Once the arthrotomy was performed, a good exposure could be obtained for the medial femoral condyle and the patient’s knee was in 90-degree flexion and off the trochlea when the knee was in extension.
The lesions were again seen. In preparation for the transplant, oval template was used for the medial femoral condyle with the knee in 90-degree flexion. The cartilage along the oval template was cut with the use of a blade followed by curette to reach a stable subchondral region.
There was some extension of the loose cartilage posteriorly, which was also excised in line with the defect. Templating of the defect was done with the use of the cover of chromic catgut. Once a good templating was done, it was taken to the back table.
The MACI autologous cultured chondrocytes on the porcine membrane were opened and dropped on the operating field and the template was used to cut the MACI with the cells facing up. Once the template was cut, the medial femoral condyle was checked for any active bleeding.
Hemostasis was achieved well. Two drops of Vista seal were put on the floor and the graft MACI was put on it with the cells facing towards the bone. The Tegaderm was removed and the MACI membrane was patted well with the use of patty gently. Three minutes were given to dry.
Vista seal was applied along the margins also. The posterior margin of the membrane was sutured to the adjacent cartilage using 6-0 Vicryl. Once it was implanted well and dried, the knee was extended to focus attention on the trochlear lesion.
An oval cutting block was again taken, small size, and put on the defect and punched enough to make an abrasion along the cartilage. Knife and curette were used to create the defect. Subchondral bone was reached. Hemostasis was induced with the use of Gelfoam-soaked thrombins.
The MACI membrane was cut with the use of the same cutting block and hammer. The cut was made with a piece of tourniquet behind it. Now the cell surface facing the bone membrane was put onto the defect after application of Vista seal.
It was allowed to dry for 3 minutes followed by application of Vista seal on the edge and again allowed to dry for 3 minutes. Once it was dried, the knee was ranged gently and the grafts were checked on both sides and found to be stable.
Knee was gently irrigated with the use of normal saline. Hemostasis was achieved and closure was done in layers using PDS 4 and 2-0 Vicryl for the arthrotomy followed by 2-0 Vicryl for subcutaneous and 3-0 Monocryl for the skin.
Dressing was done with the use of Xeroform, 4 x 8’s, ABD, Webril, Ace wrap. Knee immobilizer was applied. The patient was given a post op femoral block. The patient was extubated and went to recovery in a stable condition.
With continued physical therapy and follow up checkup the patient did well after the surgery.
Disclaimer – Patient’s name, age, sex, dates, events have been changed or modified to protect patient privacy.
