Case Study: Torn Meniscus due to Aging:
Medial Meniscus Repair and Chondroplasty
Inside your knee, two pieces of cartilage reside between your thigh bone (femur) and shinbone. (tibia). The meniscus is this tissue. The rubbery wedges of cartilage act like shock absorbers for your knee, providing cushioning for your bones and knees.
The cartilage in your knees wears down and becomes weaker as you mature. This weaker cartilage is more prone to tearing. A meniscus rupture can also be caused by arthritis (the breakdown of cartilage in the joints).
A meniscus tear is a prevalent knee injury. Meniscus tears are common in athletes and recreational players. The injury is also prevalent in older people and those with knee arthritis.
The patient is a 55-year-old female who is complaining of left knee discomfort. She has no recollection of being hurt. She started experiencing pain a year ago. The agony is excruciatingly painful. The discomfort is described as sharp by the patient.
The pain is constant and interferes with slumber. The discomfort is accompanied by swelling. Since its inception, the issue has gotten worse. Walking and standing aggravate the symptoms. Nothing alleviates the discomfort.
XR showed very mild left knee arthrosis, preferentially involving the medial compartment. Arthrosis occurs due to wear and tear of the cartilage at the joints. It usually happens because of aging or intense use of the joints during sports, exercise or other activities.
There is minimal joint space narrowing at the medial aspect of the medial femorotibial compartment. Very small marginal osteophytes are present. There is a very small left knee joint effusion.
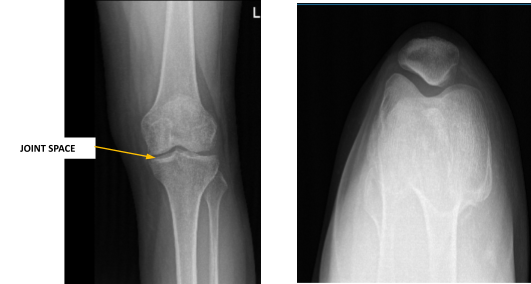
Left knee X-ray complete with patella
MRI also performed and there is an oblique tear of the body and posterior horn of the medial meniscus and found medial and patellofemoral compartment articular cartilage defects. The patella is slightly subluxed laterally relative to the femur.
Upon examination of the left knee, the patient is tender to palpation along the medial joint line, and has an effusion. Patient also has PF crepitus and tenderness on palpation along the medial and lateral PF joint line. Patellar grinding test is positive.
The patient has discomfort with McMurray’s maneuvers, and the knee is stable. They lack full flexion secondary to the effusion, but have full extension. They have 5/5 strength, and are neurovascularly intact distally. There is no erythema, warmth or skin lesions present.
On examination of the contralateral extremity, the patient is nontender to palpation and has excellent range of motion, stability and strength.
We discussed the treatment options for the patient’s diagnosis, which included: living with the extremity as it is, organized exercises, medicines, injections and surgical options. We also discussed the nature and purpose of the treatment options along with the expected risks and benefits.
The patient has expressed a desire to proceed with surgery. I educated the patient regarding the inherent and unavoidable risks which include, but are not limited to: anesthesia, infection, damage to nerves and blood vessels, blood loss, blood clots, and even death were discussed at length.
We also talked about the possibility of not being able to return to prior activities or employment, the need for future surgery, and complex regional pain syndrome.
The patient is also aware that a lengthy rehabilitative process usually follows the surgical treatment. We discussed the prospect of not being able to relieve all of the discomfort. I also stated that there is no assurance that all function and strength will be restored. We intend to perform a medial meniscectomy and a chondroplasty on the left knee.
Anesthesia was administered. After applying a mid-thigh tourniquet and using chlorhexidine paint, the left lower limb was prepared. After exsanguination, the ligature was raised to 350 Hg. The lower extremity of the 1Jft was put in a leg holder. The left lower limb was draped aseptically.
The knee scope was then inserted through a lateral working aperture in the left knee. A knee examination revealed patellofemoral arthritis, particularly in the distal medial patellar joint.
The trochlea had OA grade 1 to 2 changes, and the medial inferior patellar component had OA grade 3 to 4 changes. Chondroplasty of the inferomedial patellar aspect was combined with a medial femoral gutter synovectomy.
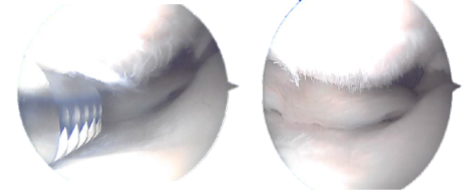
Intraoperative Arthroscopic images taken during operation
The knee was completely irrigated and shed. The knee was closed with nylon #3-0 sutures. Dry treatment was done with Adaptic, 4 x 4, and Webril. TED hose was used on the thighs. The ligature was taken off. The patient was successfully extubated.
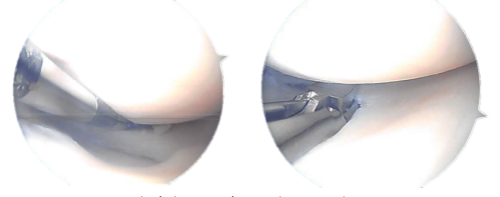
Final pictures taken during operation
After a week of recovery, the patient was seen, and an examination of the left knee revealed a tiny effusion. The wounds are mending well, with no signs of drainage, erythema, or warmth.
Because of the discomfort, there is a restricted range of motion. Distance strength is 5/5. There is no calf soreness and the Homan’s sign is negative. Distally, sensation is intact to light contact, and capillary refill is rapid.
We chose to continue with formal physical therapy as well as a home exercise program for knee rehabilitation after discussing treatment options. We will continue to use ice and elevate the leg to reduce swelling and pain.
To minimize the risk of deep vein thrombosis, we will continue to use early mobilization and mechanical prophylaxis. The patient returned to the clinic every 3-4 weeks. The patient recovered well from the surgery and proceeded with physical therapy.
Disclaimer – Patient’s name, age, sex, dates, events have been changed or modified to protect patient privacy.

Dr. Vedant Vaksha
I am Vedant Vaksha, Fellowship trained Spine, Sports and Arthroscopic Surgeon at Complete Orthopedics. I take care of patients with ailments of the neck, back, shoulder, knee, elbow and ankle. I personally approve this content and have written most of it myself.
Please take a look at my profile page and don't hesitate to come in and talk.
