Case Study: Knee Arthroscopy: Arthroscopic Chondroplasty of
the Patella and Medial Femoral Condyle in a 29-year-old male
The surgery called a knee arthroscopy uses a tiny camera to look inside your knee. A person with injured knees may develop blood clots, break off, and cause life-threatening illnesses.
This makes a person limit his/her mobility. Performing knee arthroscopy in a broken knee could potentially reduce uncomfortable signs and symptoms of a variety of conditions that harm the joint’s soft tissues and cartilage surfaces.
A 29-year-old patient visited our office with complaints regarding his left knee pain. Patient stated that he cannot put weight on knee, and the patient is also limping. The pain is mild to moderate in intensity and described the pain as sharp and dull.
The pain is intermittent and is also associated with swelling and limping but not with bruising, tingling, numbness, radiating pain, weakness, bowel or bladder abnormality, gait problem, giving way, or hand function difficulty.
The problem has been getting better since it started. Ice, knee braces, and ibuprofen make the symptoms better. The patient has undergone no surgery. Patient has no medical history. The patient is currently taking tonsil medication. Patients do not smoke.
Upon examination of the left knee, there is no ecchymosis, abrasions, or lacerations. There is a q2+ knee effusion. There is no pain with palpation along the medial or lateral border of the patella. Active range of motion is limited secondary to pain, but the patient can fully extend the knee and flex to 90 degrees.
Passive range of motion is like active. There is no crepitation throughout the range of motion. There is no pain to palpation along the medial or lateral femoral epicondyle. Palpation along the medial or lateral joint lines does not reproduce pain.
McMurray’s maneuver produces generalized knee pain but no joint line-specific pain. Collateral ligaments are intact to varus/valgus stress. There is a 3+ Lachman. Pivot shift cannot be performed secondary to pain. The posterior drawer is negative.
The Dial test is negative. There is no soft tissue swelling distally. Neurocirculatory examination is intact. On examination of the contralateral extremity, the patient is nontender to palpation and has an excellent range of motion, stability, and strength.
He presented the MRI results of his left knee and showed a small bony contusion involving the lateral proximal tibia. Large joint effusion and incomplete tear involving the lateral retinaculum at its attachment to the patella. The ACL is heterogeneous and poorly visualized indicating tear. Clinical correlation recommended.
We discussed the treatment options for the patient’s diagnosis, which included living with the extremity as it is, organized exercises, medicines, injections, and surgical options. We also discussed the nature and purpose of the treatment options along with the expected risks and benefits.
I educated the patient regarding the inherent and unavoidable risks which include, but are not limited to anesthesia, infection, damage to nerves and blood vessels, blood loss, blood clots, and even death were discussed at length.
We also talked about the possibility of not being able to return to prior activities or employment, the need for future surgery, and complex regional pain syndrome.
The patient also understands there is a long rehabilitative process that typically follows the surgical procedure. We talked about the possibility of not being able to alleviate all the discomfort.
Also, I explained there is no guarantee all the function and strength will return. The patient also understands the risks of re-tear or failure to heal.
The patient understands implants may be utilized during this surgery. The patient expressed understanding of these risks and has elected to proceed with surgery. We have discussed the surgical procedure as well as the realistic expectations regarding the risks, outcome, and post operative protocol.
The patient was taken to the operating room where he was placed on a well-padded operating room table. General anesthesia was induced. The left lower extremity was prepped and draped aseptically. Preoperative antibiotics were given. Tourniquet was elevated. Arthroscopic examination was done from the lateral entry border.
A medical entry portal was also made. There was grade 2 to grade 3 arthritis on the medial femoral condyle, which was cleaned by shaver. There was grade 2 to grade 3 arthritis on the patella, which was cleaned by the shaver, medial as well as lateral meniscus tear. Examination of the intercondylar notch there was 90% tear of the ACL, which was decided to be reconstructed and it was not repairable.
Debridement of the ACL was done. There were some fibers of the posterior ACL left intact to allow for proprioception. Quad tendon was harvested through a midline suprapatellar incision by using the quad tendon harvesting kit 8 mm x 10 mm x 75 mm of graft was repaired by putting FiberLinks on either side.
Arthroscopic ACL foot stump was performed on the medial surface of the lateral condyle of the femur as well as footprint. ACL was used to allow insertion of flip outer from the lateral femoral condyle through a small incision. A flip cutter was used to make a tunnel of about 35 mm In the femur alts.
Similarly, a filo cutter was used to make a tunnel with a tibial ACL guide on the tibial side and tunnel of 25 mm. After thorough the ACL graft was inserted using wires for shuttling into the femoral and then followed by tibia with up on either end.
The graft was tightened with a tightrope on either end and found to be in an acceptable position and checked by an arthroscope. The tightropes were tied to each other, and the shuttling suture was removed. Final pictures were taken and saved.
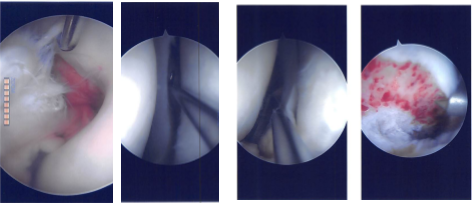
Intraoperative Arthroscopy Images
The arthroscope was removed. Closure of the knee was done after thorough Irrigation In layers using #0 Vicryl, # 2-0 Vicryl and #3-0 Monocryl. Dressing was done using 4×4, Adaptic, ABD, Webril and Ace wrap. Knee immobilizer was applied.
The patient was then extubated. Adductor canal femoral block was done by anesthesia. The patient was informed pre op as well as after the surgery that the father was informed about it. The patient was informed about the precautions and use of the knee mobilizers, ice, elevation, medications that have been given.
The patient was seen for a post operative check up. We have decided to do formal physical therapy as well as a home exercise program for rehabilitation of the knee.
The patient did well after the surgery and continued physical therapy. Patient checked in for a follow up visit after a month and saw significant improvement on his knee.
Disclaimer – Patient’s name, age, sex, dates, events have been changed or modified to protect patient privacy.
I am Vedant Vaksha, Fellowship trained Spine, Sports and Arthroscopic Surgeon at Complete Orthopedics. I take care of patients with ailments of the neck, back, shoulder, knee, elbow and ankle. I personally approve this content and have written most of it myself.
Please take a look at my profile page and don't hesitate to come in and talk.

