Case Study: Right Knee Arthroscopic Medial Meniscectomy
with Abrasion and Microfracture Chondroplasty
The knee can hold the body in an upright position without the need for muscles because of its many functionalities. enables the body to be raised and lowered. provides safety.
The lateral meniscus serves as a significant stress absorber on the lateral surface of the knee joint. That is the main reason we need to pay close attention to the health of our knees.
Patient presents bilateral knee pain. She remembered that pain started two years ago. She has done physical therapy which did not help. Then she was in pain management and gave a cortisone injection in both knees which helped for a month only.
She takes Tylenol which helps. X-ray result presented today and it clearly showed her bilateral knees have mild patellofemoral compartment osteoarthritis and small joint effusion.

We discussed treatment options including physical therapy, injection and even surgery. For now, we decided to have 3 Tesla MRIs for both knees. Patient will continue to apply ice/heat.
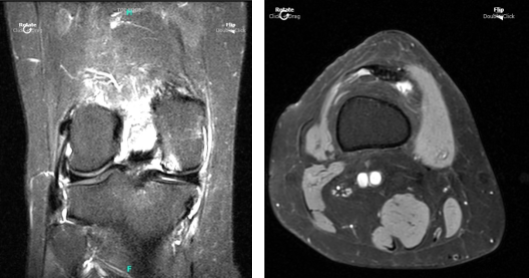
Patient returned to our office a week after the initial visit. Presented bilateral X-rays. Left knee demonstrates small full-thickness cartilage defects of the medial with inferior aspect of the lateral patellar facets with underlying patchy subchondral bone marrow edema.
Small partial-thickness cartilage defects on the medial trochlear facet. Small partial thickness cartilage loss central aspect of the medial femoral condyle with underlying small faint subchondral bone marrow edema. Small joint effusion and intact cruciate and collateral ligaments.
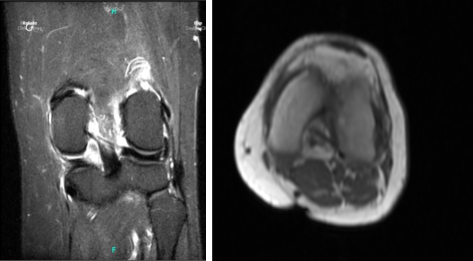
Her MRI right knee showed impression as follows: full-thickness cartilage defect inferior aspect of the lateral patellar facet and small full-thickness cartilage fissures of the medial patellar facet with underlying subchondral bone marrow edema.
Small full-thickness cartilage fissure of the medial trochlear facet with underlying small subchondral edema. Small full-thickness cartilage defects central aspect of the medial femoral condyle with underlying small subchondral bone marrow edema. Small to moderate joint effusion. Trace popliteal cyst.
The patient was taken to the operating room after an informed consent. General anesthesia was induced. The right thigh was prepped and draped aseptically in the usual fashion after application of the tourniquet.
The tourniquet was elevated to 300 mmHg after injection of 2 grams of Ancef as preoperative antibiotics. A time-out was called. A lateral entry portal was made and a scope was entered.
A medical entry portal was made with the use of a spinal needle. Examination of the medial tibiofemoral compartment showed fraying of the lateral free margin of the medial meniscus along with undersurface flap tear of the body of the medial meniscus.
There was grade 3 to grade 4 osteochondral damage of the weightbearing surface of the medial femoral condyle. Debridement of the meniscus as well as the cartilage was done with the use of a shaver.
Abrasion chondroplasty was done with a shaver, followed by microfracture of the bare bone with use of the chondral pick set on the femoral condyle. Examination of the intercondylar notch showed intact ACL. Examination of the lateral tibiofemoral compartment showed intact meniscus and cartilage.
Examination of the patellofemoral compartment showed denudation and fraying of the cartilage of the inferior surface of the patella, which was debrided with the use of shaver. Abrasion chondroplasty was performed with the use of a shaver.
The arthroscope was then inserted through the medial entry portal and the shaver was inserted through the lateral entry portal, and further debridement of the meniscus and cartilage was performed. Final pictures were saved. The knee was thoroughly irrigated and drained. Blood could be seen coming out of the microfracture sites. Closure was done with the use of 3-0 nylon.
Then, 30 mL of 0.5% Marcaine mixed with 40 mg of Depo-Medrol was injected into the knee. The dressing was done with the use of Adaptic, 4×4, ABD, Webril and Ace wrap. The tourniquet was removed. The patient was extubated and moved to recovery in a stable condition.
After a week, the patient was seen for post-operative checkup. She denies fever and chills. Pain is well controlled. Post Operative Exam: General Appearance: swelling and tenderness and wound clean and dry, no warmth, appropriate range of motion, and neurovascular intact.
We discussed treatment options for fast recovery including conservative management like RICE Therapy (Rest, Ice, Compression and Elevate), Injection, and physical therapy.
By this time the patient decided to take the conservative manner. With consistent visits every four weeks, the patient saw a significant recovery from her surgery and was able to return to her normal routine.
Disclaimer – Patient’s name, age, sex, dates, events have been changed or modified to protect patient privacy.

Dr. Vedant Vaksha
I am Vedant Vaksha, Fellowship trained Spine, Sports and Arthroscopic Surgeon at Complete Orthopedics. I take care of patients with ailments of the neck, back, shoulder, knee, elbow and ankle. I personally approve this content and have written most of it myself.
Please take a look at my profile page and don't hesitate to come in and talk.
