Case Study: Management of Tendoachilles
Rupture in a 35-year-old BasketBall Player
A 35-year-old female basketball player presented one day after sustaining an injury to the right ankle while playing. The patient reports she heard a popping sound while jumping during the game. She immediately felt pain and swelling in the right ankle with difficulty walking.
The patients applied icing on the right ankle and used pain medication in the form of ibuprofen. The patient denies any use of any current medication. The patient is a nonsmoker and denies any use of illicit drugs. The patient denies any known drug allergies.
On physical examination of the right ankle, a palpable gap was present 5 cm above the calcaneal insertion of the Tendon Achilles. The dorsiflexion of the right ankle was normal however the plantar flexion was absent. Thompson’s test, squeeze test, and matles test were positive.
An MRI of the right ankle showed a complete tear of the right Tendon Achilles. The rupture was through the watershed zone. The patient was advised operative repair of the torn tendon. The risks, benefits, and complications of surgery were explained at length to the patient. The patient verbalized agreement and signed the informed consent.

Intraoperative picture of the Tendoachilles repair.
PREOPERATIVE DIAGNOSIS: Tendo Achilles tendon rupture of the right side.
POSTOPERATIVE DIAGNOSIS: Tendo Achilles tendon rupture of the right side.
OPERATION: Open Tendon Achilles repair.
DESCRIPTION OF PROCEDURE: The patient was taken to the operating room where general anesthesia was induced. The patient was intubated and turned prone in a well-padded position. All the bony prominences were well padded. The right lower extremity was prepped and draped aseptically in the usual fashion. A thigh tourniquet was applied. The preoperative antibiotic was given. Tourniquet was inflated. A time-out was called.
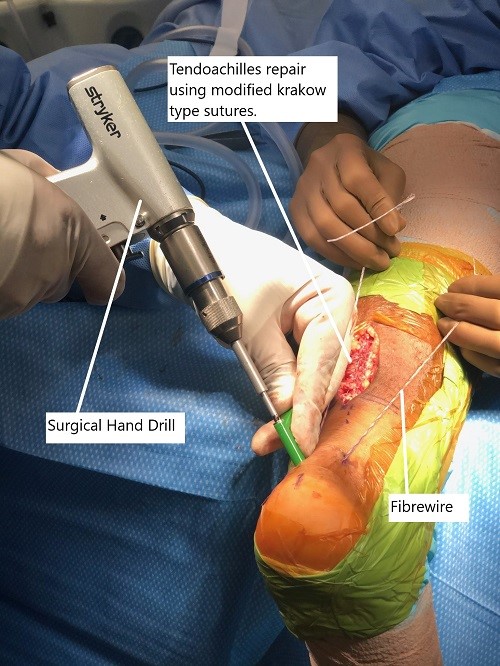
Intraoperative image showing the Tendon Achilles repair.
An incision was given medial to the midline, which is two-thirds superior and one-third inferior to the gap in the Tendon Achilles. With sharp dissection, the paratenon was reached and incised along the line of the incision. Complete tear of the tendon Achilles would be seen. Proximal modified Krackow-type sutures were planned and two SutureTapes were used to do the modified Krackow stitch with the prior chosen site.
The four tails were retrievable on the inferior end of the stump. The distal stump was cleaned. Two distal incisions were given over the calcaneum on either side of the insertion of the tendon Achilles. The Banana suture retriever was passed through the incision along the tendon Achilles proximally on either side and the two FiberWires were retrieved on either side.
SwiveLock 4.75 mm was planned with a drill at 45 & 45 degree angle lateral to the tendon Achilles insertion and into the calcaneum on either side followed by tapping and insertion of the SwiveLock.
The sutures were tensioned with the foot in plantar flexion on either side and the SwiveLock was tightened. A good repair could be seen. The repair was augmented using #3-0 FiberWire at the stump. The paratenon was closed over the repair. The closure was performed using #0 Vicryl, #2-0 Vicryl, and Monocryl.
The SwiveLock incisions were closed using #0 Vicryl and #4-0 nylon. The wound was washed prior to closure. The dressing was performed using 4x8s, ABD, Webril, posterior splint in plantar flexion. The patient was turned into the bed and extubated and moved to recovery in a stable condition. An above-knee plaster cast was applied in plantar flexion.
The plaster cast was cut in 2 weeks and a below-knee plaster cast was applied in gravity plantar flexion. At 3 weeks the cast was removed and the patient was put in a walking cast with heel wedges which were removed sequentially.
Partial weight-bearing was allowed and gentle progressive active range of motion exercises was started. Patient was full weight bearing and had good range of movement at 8 weeks after the surgery.
Disclaimer – Patient’s name, age, sex, dates, events have been changed or modified to protect patient privacy.

Dr. Suhirad Khokhar
My name is Dr. Suhirad Khokhar, and am an orthopaedic surgeon. I completed my MBBS (Bachelor of Medicine & Bachelor of Surgery) at Govt. Medical College, Patiala, India.
I specialize in musculoskeletal disorders and their management, and have personally approved of and written this content.
My profile page has all of my educational information, work experience, and all the pages on this site that I've contributed to.
