Case Study: A 65 year-old female
underwent Arthroscopic Rotator Cut Repair
Acromioplasty, and Extensive Debridement
The rotator cuff is made up of muscles and tendons that help to keep the shoulder in position. It is one of the most vital components of the shoulder. It enables you to raise your arm and grasp upward.
A rotator cuff injury, such as a tear, can occur abruptly when falling on an outstretched hand or develop over time as a result of repetitive activities. Aging can also induce rotator cuff degeneration and tears.
If your rotator cuff is injured, you may need surgery to fix it. Shaving off bone spurs that are pinching the shoulder or mending torn tendons or muscles in the shoulder are examples of procedures that may be performed.
A rotator cuff tear can be repaired surgically using arthroscopy, open surgery, or a mix of the two. The aim of rotator cuff repair surgery is to help restore the function and flexibility of the shoulder while also relieving pain that other treatments cannot control.
The patient is being seen for left shoulder and neck discomfort. She was in a car mishap five years ago, but the pain is still present. Her pain is constant, dull, and stabbing, and it worsens with exercise. It also disturbs her slumber. She has spasms and tightening, and she is perpetually tense.
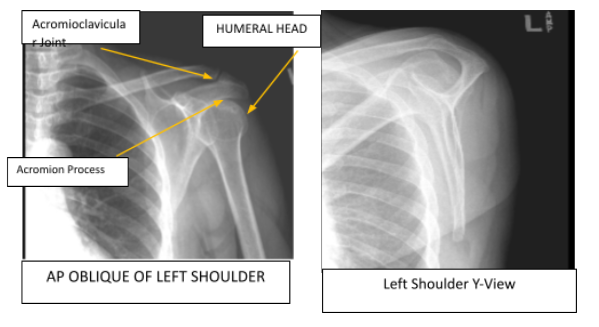
MRI showed a high grade partial tear of supraspinatus along with tendinopathy of the infraspinatus. Found 4-mm cyst in the humeral head supraspinatus tendinopathy and fraying 10 mm x 9 mm high-grade articular and interstitial tear at the anterior insertion.
We went over treatment choices, including injection, surgery, and physical therapy. The patient understands the risks including but not limited to infection, stiffness, deep various thrombosis, persistent or worsening pain, loosening of the implant, bleeding possibly requiring transfusion, nerve or vascular injury, instability, loss of sensation, mortality. We talked about the possibility of RC repair and the chance of failure after surgery when continuing smoking.
The patient was aware of the risks and advantages. We discussed going ahead with surgery. We talked about extended rehabilitation and other issues. Arthroscopy and shoulder debridement with possible rotator cuff repair, acromioplasty, and distal clavicle resection were decided upon by the patient.
A preparatory brachial block was performed. Patient was positioned laterally using a bean bag positioner. Chlorhexidine was applied to the left shoulder and permitted to sit for 3 minutes.
Draping was done on the left shoulder, and the left upper extremity was hung over a pulley with a 10-pound weight. A posterior portal was created to allow for a tiny incision along the posterior glenohumeral joint and the introduction of a scope.
Anterior portal was created using spinal needle localization, incision, and a trocar. Glenohumeral joint showed osteoarthritis of the humeral head of grade 3 to grade 4 with cartilage flaps and fraying of the labrum. A high-grade partial-thickness tear of the infraspinatus behind the biceps tendon could be identified.

The loose chondral flaps were shaved and the labrum was debrided. A PDS was passed over a spinal needle through the rotator cuff tear for localization. The debridement of cartilage flap was performed through the posterior working portal. Extensive bursitis was present and subacromial was removed and bursectomy performed.
The acromion was repaired and acromioplasty was performed. PDS identified, rotator cuff tear was prepared and the bone was abraded. Posterolateral portal was made in line with the tear for passage of sutures into the rotator cuff from an anchor and tied with a knot. The knot was tied from a superior portal.
Final pictures were taken and the shoulder was drained. The portals were closed using nylon. Dressing was done using Adaptic, 4×4, ABD, and tape. The patient was moved to the post-operative holding area. The patient tolerated the procedure well.

After a week, examination of the left shoulder reveals that the incisions are well healed, without evidence of drainage, erythema or warmth. Range of motion and strength are progressing appropriately at this stage of rehabilitation.
Strength remains 5/5 distally. There is no tenderness at the elbow and wrist. Sensation is intact to light touch distally and there is a brisk capillary refill.
Patient chose to continue with a home exercise program for shoulder rehabilitation after discussing treatment options. She continued to apply ice to the shoulder and elevate it, as well as take pain medicine, to reduce swelling and pain.
To decrease the chances of a deep vein thrombosis, the patient will continue to use early mobilization and mechanical prophylaxis. Every 3-4 weeks, the patient returned to the clinic. The patient recovered well from the surgery and continued physical rehabilitation.
Disclaimer – Patient’s name, age, sex, dates, events have been changed or modified to protect patient privacy.

Dr. Vedant Vaksha
I am Vedant Vaksha, Fellowship trained Spine, Sports and Arthroscopic Surgeon at Complete Orthopedics. I take care of patients with ailments of the neck, back, shoulder, knee, elbow and ankle. I personally approve this content and have written most of it myself.
Please take a look at my profile page and don't hesitate to come in and talk.
