Total Hip Joint Dislocation
Hip replacement surgery provides relief from chronic hip pain caused by arthritis and other diseases. Patients return to the activities they enjoy benefiting from increased mobility.
Although total Hip replacement remains one of the most successful surgeries in modern medicine, not all patients have perfect outcomes.
One of the dreaded complications of hip replacement surgery is dislocation. Hip dislocation is uncommon but may occur in about 2% of patients, mostly within the first year of the surgery. Dislocation rates are significantly higher in revision surgeries.
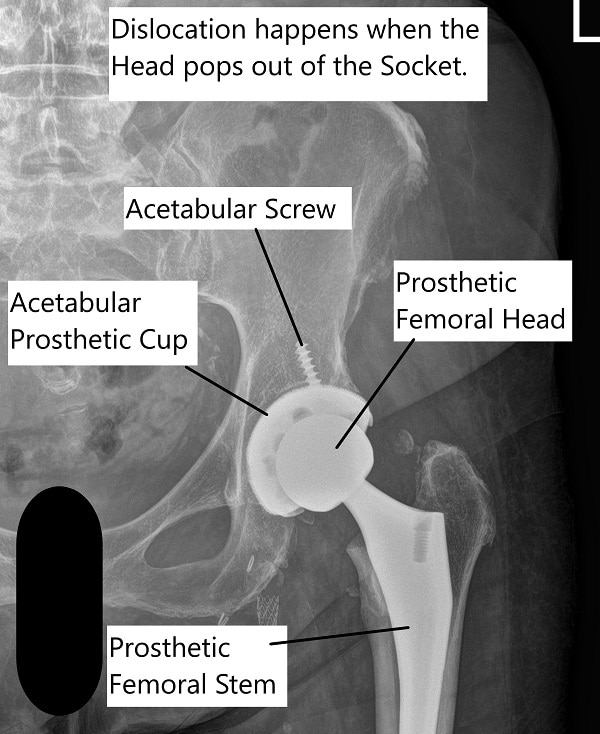
A dislocation occurs when the ball of the prosthetic implant is pushed out of the socket. The hip replacement performed through the anterior approach is more vulnerable to anterior dislocation. Similarly, the hip replacement performed utilizing the posterior approach is more vulnerable to posterior dislocation.
Total Hip Replacement and Dislocation
Total hip replacement is a surgery to replace the diseased parts of the hip joint with prosthetic parts. The surgery involves duplicating the function as well as balancing the muscular forces acting around the joint. Due to the unique biomechanics of the natural hip joint, the artificial joint needs to be placed in a proper position.
The hip joint is a large weight-bearing ball and socket joint. The ball is formed by the upper part of the thigh bone. The ball fits into the socket formed by the lower part of the pelvis. Hip replacement is commonly performed for arthritis after all conservative treatment options have been exhausted.
The joint is covered by a tough tissue known as a joint capsule, which seals the joint stabilizing it. The joint is also covered by ligaments and muscles which hold the joint in place. Together these structures keep the ball in the socket, preventing dislocation. The alignment of the natural hip further adds to its stability.
Hip replacement loosens the soft tissues around the joint, and patients are advised hip precautions to prevent dislocation. These are the movements and maneuvers the patients are advised to avoid. Certain positions may put the hip ball (femoral head) in a position where it may pop out of the socket.
Total Hip Arthroplasty dislocation
Some of the common precautions are:
- Not to bend your thigh more than 90 degrees
- Not to sit in low chairs/sofas/toilet seats
- Not to cross legs
- Not to sleep on the side
These precautions are especially important in the traditionally performed posterior hip approach (from behind the hip). The hip precautions are practiced together with an abduction pillow for a few weeks after the surgery.
Symptoms and Causes
Often the patients report hip dislocation immediately as difficulty moving the Hip. Patients are unable to bear weight on the side involved without pain.
Various factors are involved in the incidence of hip dislocation after the surgery. The treated patients may feel anxious about hip movement as they are apprehensive about dislocation. They may patient factors or procedure factors.
Patient factors
Patient age plays an important factor in the risk of prosthetic hip dislocation. Older patients may sustain dislocation secondary to falls/trauma due to an increased risk of loss of balance. Patients in higher age groups are also less likely to be compliant with hip precautions.
Prior surgeries of the hip joint make it more vulnerable for dislocation after replacement. As with any surgical procedure, there may be a residual loosening of the tissues around the joint. Laxity of tissues supporting the hip joint makes it more vulnerable to dislocation.
Neuromuscular conditions such as Parkinson’s diseases, cerebral palsy, etc may make the patient prone to sustain a dislocation following surgery. Neuromuscular conditions render the muscle groups either spastic or paralytic contributing to instability and dislocation.
Developmental hip disorders such as hip dysplasia make the hip more prone to dislocation. The shallow acetabular cup and tightened or lax structures around the hip joint contribute to instability and dislocation.
Patients suffering from obesity and other medical conditions such as diabetes are more likely to sustain a dislocation after replacement surgery. The increased risk is attributed to the neurological deficit in limbs, loss of balance, and greater chances of infection.
Procedure factors
The posterior surgical approach (from behind) involves cutting the muscles and stabilizing structures. This makes the hip more vulnerable to posterior dislocation compared to the muscle-sparing anterior approach (from the front).
Implant position is an important factor in hip dislocation following replacement. The proper position of the components during surgery is vital for keeping the ball in the socket.
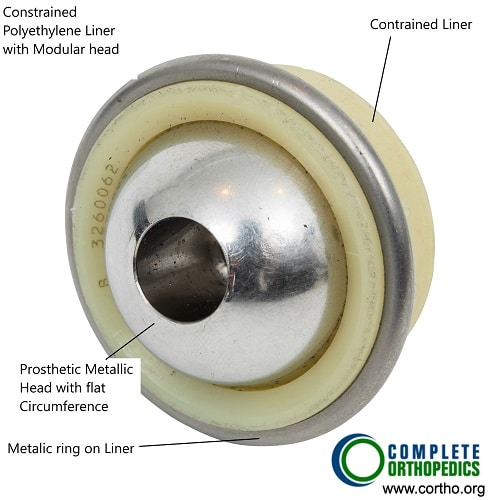
Constrained Liner
A constrained liner consists of a polyethylene liner containing the head of the femur. The head of femur while being contained in the socket does not dislocate. The constrained design may however increase the wear and tear of the implants.
The surgeon’s experience in performing the surgery through a particular approach reduces the risk of dislocation.
The choice of implant used reduces the incidence of dislocation episodes. During the past decade, the size of the head of the femur in implants has increased considerably. Larger head means a larger range of motion before dislocation.
Diagnosis and Management
Hip dislocation following replacement is evident with the symptoms experienced by the patients. Most patients report to the ER following an episode of dislocation. The patients are subjected to imaging such as X-Ray or CT scan (computed tomography).
Nonsurgical
A procedure called hip reduction is done which involves placing the ball back into the socket of the pelvis. It is generally done under moderate sedation or under anesthesia in the operating room. Once the reduction is achieved the hip is placed in a brace for several weeks. Subsequent risks of dislocation remain high in case the dislocation is due to unaligned implants.
Surgical
Multiple episodes of dislocation and dislocations due to implant alignment issues may require revision hip replacement surgery to place the components correctly. Special implants may be used to prevent future dislocations. The socket cup and femoral stem may be repositioned to achieve correct alignment.
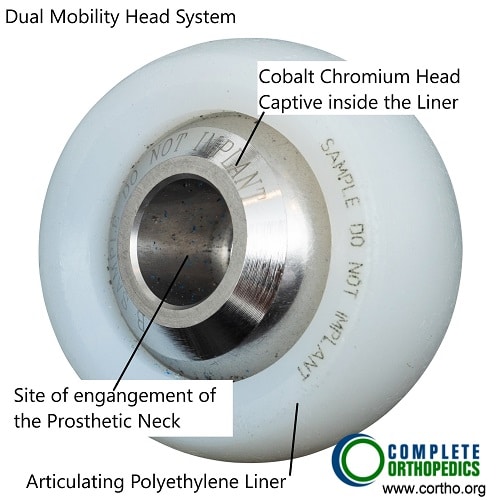
Dual mobility head and liner
Dual mobility head and liner utilizes a articulating small head held captive in the liner, the liner articulates inside the acetabular shell. The design ensures stability of the head while allowing greater movement of the prosthetic hip.
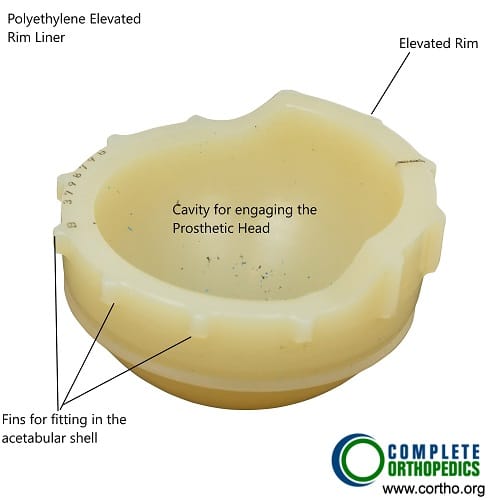
Acetabular liner with elevated lip
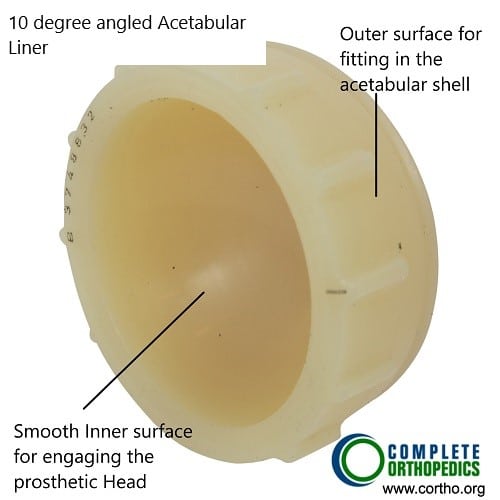
10 Degree angled acetabular liner
Specially designed acetabular liners with elevated lip or lateralization creates a deeper cavity for the head of the femur before it can pop out of the socket. The special design while allowing stability also does not restrict the range of motion of the head of the femur.
Recently specially designed implants are available to prevent the dislocations. Innovations in increasing head size and dual mobility of the implant cups are promising options for reducing the risks of dislocations. Robotic-assisted hip replacements promise accurate implant positioning. The choice of implant, the approach of surgery, and surgeon experience are factors important in reducing the risk of dislocation.
Do you have more questions?
What are the risk factors for total hip joint dislocation?
Risk factors for total hip joint dislocation include advanced age, previous hip surgeries, congenital hip abnormalities, and certain medical conditions affecting joint stability.
Can total hip joint dislocation occur spontaneously, without any traumatic event?
While uncommon, total hip joint dislocation can occur spontaneously in individuals with certain predisposing factors such as ligamentous laxity or muscle weakness.
What are the symptoms of total hip joint dislocation?
Symptoms of total hip joint dislocation include severe pain, inability to bear weight on the affected leg, visible deformity or abnormal positioning of the hip, and limited range of motion.
Is total hip joint dislocation a medical emergency?
Yes, total hip joint dislocation is considered a medical emergency that requires immediate evaluation and treatment to prevent complications such as nerve or blood vessel injury.
What complications can arise from total hip joint dislocation?
Complications of total hip joint dislocation may include nerve damage, vascular injury, fracture of the hip socket or femur, avascular necrosis of the femoral head, and long-term joint instability.
What is the typical treatment approach for total hip joint dislocation?
The treatment of total hip joint dislocation often involves closed reduction, where the hip joint is manually manipulated back into its normal position under anesthesia. In some cases, surgical intervention may be necessary to stabilize the joint.
How successful is closed reduction in treating total hip joint dislocation?
Closed reduction is often successful in restoring normal hip joint alignment and function, especially when performed promptly after the dislocation occurs. However, the success rate may vary depending on factors such as the severity of the dislocation and associated injuries.
Can total hip joint dislocation lead to chronic hip instability or recurrent dislocations?
Yes, untreated or inadequately managed total hip joint dislocation can lead to chronic hip instability or recurrent dislocations, especially in cases where there is underlying ligamentous laxity or structural abnormalities.
What is the role of physical therapy in the rehabilitation of total hip joint dislocation?
Physical therapy plays a crucial role in the rehabilitation of total hip joint dislocation by restoring strength, range of motion, and stability to the hip joint, as well as addressing any residual muscle weakness or imbalances.
Are there any restrictions or precautions that should be followed after experiencing a total hip joint dislocation?
Yes, individuals who have experienced a total hip joint dislocation may be advised to avoid certain activities or movements that could place excessive stress on the hip joint, such as high-impact sports or activities that involve extreme ranges of motion.
How long does it take to recover from a total hip joint dislocation, and what is the expected timeline for return to normal activities?
The recovery time for a total hip joint dislocation depends on factors such as the severity of the dislocation, associated injuries, and the individual’s overall health. Rehabilitation and return to normal activities may take several weeks to months.
Can total hip joint dislocation lead to long-term complications such as hip arthritis?
Yes, total hip joint dislocation can increase the risk of long-term complications such as hip arthritis due to damage to the cartilage and supporting structures of the joint.
How does the age of the individual impact the treatment and prognosis of total hip joint dislocation?
The age of the individual can influence the treatment approach and prognosis of total hip joint dislocation, with younger patients often having a better chance of full recovery and lower risk of long-term complications.
Can total hip joint dislocation affect mobility and independence in daily activities?
Yes, total hip joint dislocation can significantly affect mobility and independence in daily activities, particularly if there are associated injuries or complications that limit hip function.
Are there any measures that can be taken to prevent total hip joint dislocation in individuals at risk, such as those with hip dysplasia?
Individuals at risk of total hip joint dislocation, such as those with hip dysplasia, may benefit from lifestyle modifications, physical therapy, and orthopedic interventions aimed at improving hip stability and preventing traumatic injuries.
How does the presence of other medical conditions, such as osteoporosis or rheumatoid arthritis, affect the management of total hip joint dislocation?
Other medical conditions such as osteoporosis or rheumatoid arthritis may complicate the management of total hip joint dislocation by increasing the risk of fracture or affecting bone healing. Close coordination with other specialists may be necessary for comprehensive care.
Can total hip joint dislocation cause damage to surrounding structures such as nerves or blood vessels?
Yes, total hip joint dislocation can cause damage to surrounding structures such as nerves or blood vessels, especially if the dislocation is severe or if there are associated fractures.
How does the mechanism of injury influence the severity and treatment of total hip joint dislocation?
The mechanism of injury, such as the direction and force of impact, can influence the severity and treatment of total hip joint dislocation. For example, high-energy traumas may result in more extensive soft tissue damage and require surgical intervention for stabilization.
Can total hip joint dislocation affect other joints or areas of the body, such as the lower back or knees?
Yes, total hip joint dislocation can affect other joints or areas of the body indirectly through compensatory movements or altered biomechanics, potentially leading to secondary pain or dysfunction. Rehabilitation and addressing underlying issues are important for overall recovery and function.

Dr. Suhirad Khokhar
My name is Dr. Suhirad Khokhar, and am an orthopaedic surgeon. I completed my MBBS (Bachelor of Medicine & Bachelor of Surgery) at Govt. Medical College, Patiala, India.
I specialize in musculoskeletal disorders and their management, and have personally approved of and written this content.
My profile page has all of my educational information, work experience, and all the pages on this site that I've contributed to.
