Case Study: Management of shoulder impingement
syndrome with AC arthritis in a 55-year-old female
A 55-year-old female patient presented to our office with complaints of left shoulder pain. The patient was involved in a motor vehicle accident two years ago. The pain in the left shoulder started after the accident and she received three cortisone shots in the shoulder that helped her for a few months.
Recently, the patient has had a significant limitation of daily activities secondary to shoulder pain. The patient states she experiences pain and stiffness while performing activities such as combing hair, wearing clothes, taking a shower, and driving.
The patient describes the pain as constant and sharp in character. Currently, she rates her pain as 7/10 and states the intensity as severe. She has previously tried physical therapy, hot and cold therapy, and pain injections. She takes Tylenol as needed but has not been taking any NSAIDs due to allergy.
The patient previously worked as a wrestling coach but is currently not working. She states the pain disturbs her sleep and the pain is getting worse since it started. The patient’s current medical history is significant for diabetes mellitus and hypertension controlled with medications. Previously she had a laparoscopic cholecystectomy and right shoulder arthroscopic surgery.
On examination of the right shoulder, there is no shoulder girdle atrophy. There is no soft tissue swelling, ecchymosis, abrasions, or lacerations. Active and passive range of motion is full with forwarding flexion, lateral abduction, and external rotation, though is associated with pain at the extremes of movement. Internal rotation is to the upper lumbar level with a negative lift-off sign.
The passive range of motion is full with a negative impingement sign and a negative Hawkins sign. Rotator cuff strength with forwarding flexion, lateral abduction, and external rotation is intact with 5/5 strength. There is no crepitation about the joint. Palpation of the AC joint produces discomfort and pain.
There is pain with cross-body adduction. The strength of the extremity is 5/5 at biceps/triceps/wrist extension. DRT’s are intact at +2/4 and symmetrical. The cervical range of motion is full with no pain to palpation along the paraspinal musculature medial border of the scapula. Spurling’s sign is negative.
Forward Flexion (Normal – 180 degrees) – 160 degrees
Extension (Normal – 50 degrees) – 50 degrees
Abduction (Normal – 180 degrees) – 160 degrees
Adduction (Normal – 50 degrees) – 40 degrees
Internal Rotation: upto TL junction
External rotation: 60 degrees
Upon examination of the left shoulder, the patient sits with the scapula protracted and depressed. They are tender to palpation over the anterior supraspinatus and proximal biceps. There is mild palpable crepitus in the subacromial space with ranging. The patient has discomfort with impingement maneuvers and Whipple testing.
The shoulder is stable on the exam. They have 5/5 strength and are neurovascularly intact distally. There are no erythema, warmth, or skin lesions present. Tinel’s sign over the ulnar nerve at the elbow is positive. Tenderness over the medial condyle as well as biceps tendon. Painful to flex the elbow against resistance.
Forward Flexion (Normal – 180 degrees) – 150 degrees
Extension (Normal – 50 degrees) – 50 degrees
Abduction (Normal – 180 degrees) – 150 degrees
Adduction (Normal – 50 degrees) – 40 degrees
Internal Rotation: upto TL junction
External rotation: 60 degrees
The patient was seen at the outpatient office multiple times and had cortisone injected in the left shoulder but the relief did not last long. After discussion of all treatment options and the patient opted for surgical management. The risks and benefits including infection, bleeding, injury to adjacent nerves and vessels, the possibility of repeat injection, the possibility of shoulder pain, and the need for cortisone injections among others. The patient understood and signed the informed consent.
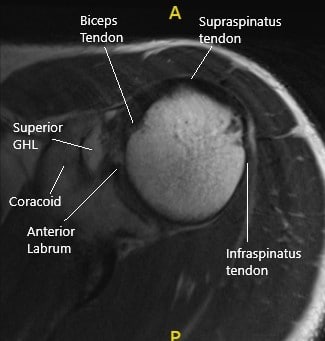
MRI of the left shoulder in axial section.
PREOPERATIVE DIAGNOSIS: Left shoulder impingement syndrome with AC arthritis.
POSTOPERATIVE DIAGNOSES:
- Left shoulder subacromial bursitis and acromial spurring left shoulder.
- Acromioclavicular degenerative arthritis left shoulder.
- Labral fraying left shoulder.
OPERATION:
- Limited debridement of the left shoulder.
- Subacromial decompression and acromioplasty left shoulder.
- Distal clavicle excision left shoulder.
DESCRIPTION OF PROCEDURE: The patient was taken to the operating room where he was placed on a well-padded operating room table. General anesthesia was induced. He was turned in the right lateral position so that the shoulder was up. The left shoulder was prepped and draped aseptically in the usual fashion. The left shoulder was put into 40 degrees of abduction and 10 degrees of flexion. A time-out was called. A perioperative antibiotic was given.

Intraoperative image of the surgical prep of the left shoulder.
The anterior portal was made posteriorly through a soft shoulder sport. The glenohumeral joint was reached and entry into the anterior portal was made using a spinal needle. The glenohumeral joint was examined. Subscapularis, suprascapular, infrascapularis, and biceps tendon were intact. There was no arthritic change in the glenohumeral joint. There was fraying of the glenoid labrum, which was cleaned using a shaver. There was no articular side rotator cuff tear.
The scope was entered into the subacromial region. Bursitis was present. The shaver was used to clean off bursitis. There was some subacromial spurring which was cleaned by using bur and doing subacromial acromioplasty. The rotator cuff was examined and this was found to be intact. Pictures were taken.
There was arthritis of the AC joint. The decision for distal clavicular excision was taken. The distal clavicular excision was performed using the bur from the posterior portal as well as the anterior portal. A centimeter of the distal clavicle was excised. Final pictures were taken and saved. The shoulder was thoroughly irrigated and drained.
The closure was done using #3-0 nylon. Local was injected onto the incision sites. The dressing was done using Xeroform, 4 x 4, ABD, and tapes. The patient was put in a shoulder sling. The patient was extubated and moved to recovery in a stable condition.
The patient had an excellent recovery post-op. A dedicated physical therapy regimen was started. The patient had an excellent range of motion free from pain 2 months following the surgery.
Disclaimer – Patient’s name, age, sex, dates, events have been changed or modified to protect patient privacy.

Dr. Suhirad Khokhar
My name is Dr. Suhirad Khokhar, and am an orthopaedic surgeon. I completed my MBBS (Bachelor of Medicine & Bachelor of Surgery) at Govt. Medical College, Patiala, India.
I specialize in musculoskeletal disorders and their management, and have personally approved of and written this content.
My profile page has all of my educational information, work experience, and all the pages on this site that I've contributed to.
