Case Study: Management of Fracture Dislocation of the
Glenohumeral Joint and Comminuted Fracture of the Shaft of Humerus
The patient is a 62-year-old female who presented to the hospital with pain, swelling, and loss of function of the left shoulder and arm. The patient had a slip and fall in the bathroom and was rushed to the hospital. She had no loss of consciousness or any ENT bleed.
She has a history of osteoporosis on treatment with alendronate, calcium, and vitamin D. Her surgical history is significant for hysterectomy done for uterine adenomyosis. She is a former smoker with a history of 20 pack years. She denied any known drug allergies.

Pre-operative x-ray of the left shoulder in AP view.
On physical examination of the left upper extremity, there was swelling and tenderness at the left shoulder and mid-arm. There was crepitus, bruising and abnormal movement of the left arm. The radial and ulnar pulses were good volume and palpable at the wrist. The neurological examination of the radial nerve, ulnar and median nerve was normal.
The x-ray revealed a spiral fracture of the proximal shaft of the humerus with dorsal angulation at the fracture site. There was a fracture of the surgical neck of the humerus with a fracture of the greater tuberosity. A CT scan of the left shoulder revealed a comminuted left humeral head fracture with anterior inferior dislocation of the main fracture fragment including the humeral head.
A large comminuted fragment remains in the vicinity of the glenoid. A small linear fragment is noted between the humeral head and left scapula. There is a major separate fracture component of the proximal humeral diaphysis with inferior angulation.
Various treatment options were discussed at length with the patient. An extensive discussion was held regarding the need for closed reduction versus open reduction of the glenohumeral joint and regarding the need for fixation of the humerus via open reduction as needed.
The patient understood the risks and benefits and complications including infection, bleeding, nonunion, malunion, need for repeat surgery, shoulder stiffness, neurological deficit, injury to adjacent nerves and vessels, weakness of the shoulder, need for repeat surgery, implant failure, fracture failure, systemic complications including pulmonary, neurological, cardiac complications among others. The patient understood and signed the informed consent.
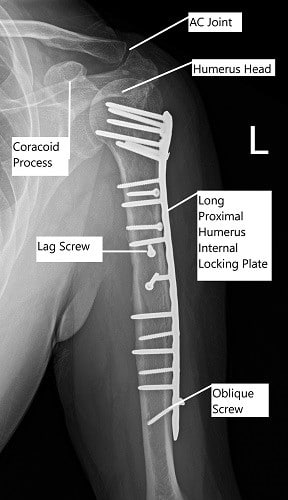
Post-operative x-ray of the left shoulder in AP view.
PREOPERATIVE DIAGNOSES:
- Fracture, midshaft of the humerus.
- Fracture dislocation of the glenohumeral joint.
POSTOPERATIVE DIAGNOSES:
- Comminuted fracture of the shaft of the humerus.
- Fracture dislocation of the glenohumeral joint of the left shoulder.
OPERATION:
- Open reduction of the glenohumeral joint.
- Open reduction and internal fixation of the greater tuberosity and shaft of the humerus using a proximal humeral plate, 14 holed, Stryker.
- Repair of the subscapularis tendon,
- Repair of the pectoralis major,
- Repair of the deltoid tendon.
- Use of intraoperative fluoroscopy.
PROCEDURE: The patient was brought to the operating room where general anesthesia was induced. A closed reduction of the glenohumeral joint through multiple maneuvers was attempted. X-ray after attempt showed extension of shaft fracture into the head, with comminution.
Further attempts were not done. A decision for open reduction and internal fixation was taken. The left upper extremity was prepped and draped aseptically in the usual fashion. The preoperative antibiotic was given. Time-out was called.
A deltopectoral approach was planned. The incision was given lateral to the subcoracoid process extending along the deltopectoral groove distally, lateral to the biceps, and along the anterolateral arm up to about 10 cm proximal to the elbow.
With sharp and blunt dissection and achieving hemostasis using Bovie, the deltopectoral approach was created. Further dissection was done laterally to the biceps. The brachialis was exposed. Further down, along the surgery, the brachialis muscle was split in the midline anteriorly to make way to the bone.
All the fractures were open. For making an approach to the humeral head and thus reduction with manipulation, the pectoralis major and then, subscapularis was raised from the humerus and the fracture fragment. The deltoid also was raised to allow fixation. The humeral head was reduced after manipulation with a pop.
After reduction of the glenohumeral joint was done, the fragments were reduced to each other with one fragment at a time, fixated with interfragmentary screws. A chunk of cancellous bone was freed from the humeral neck which was removed and morselized to be used later as a bone graft. The fractures and greater tuberosity were reduced.
A lateral plate was templated. A lateral plate template was used to find that needed a 14-hole plate (2.8 mm). A 14-hole plate was opposed laterally and then, the K-wire advanced. X-ray showed good reduction and opposition. The plate was fixed distally using cortical screws.
Following that, the humeral head was fixed using multiple locking screws. Distal fixation in the mid and distal shaft was completed with a combination of locking and non-locking screws. Pictures were taken and checked and found to be satisfactory.
The wound was thoroughly irrigated throughout the surgery as well as at the end of the surgery with copious normal saline. The subscapularis muscle, pectoralis major muscle, and deltoid muscle were repaired back to the bone and the plate using fiberwise No 2. A local bone graft was put. Final pictures were taken and saved.
Bone graft was put around the fracture site. A 2 g of vancomycin was sprinkled over the wound. The closure was done in layers using Vicryl #1, Vicryl #2, Vicryl #2-0, and staples. The dressing was done using Aquacel. The patient was extubated and moved to recovery in stable condition.
She had been healing well and is able to regain a good range of motion and strength and is back to preoperative activity with minimal restrictions.
Disclaimer – Patient’s name, age, sex, dates, events have been changed or modified to protect patient privacy.

Dr. Suhirad Khokhar
My name is Dr. Suhirad Khokhar, and am an orthopaedic surgeon. I completed my MBBS (Bachelor of Medicine & Bachelor of Surgery) at Govt. Medical College, Patiala, India.
I specialize in musculoskeletal disorders and their management, and have personally approved of and written this content.
My profile page has all of my educational information, work experience, and all the pages on this site that I've contributed to.
