Case Study: Knee Arthroscopy: ACL Reconstruction using
Quadriceps Autograft with Medial and Lateral Meniscectomy
and Chondroplasty in 20 year-old young male
Quadriceps ACL Reconstruction under general anesthesia, an autograft is a minimally invasive arthroscopic technique and a surgical treatment that replaces or reconstructs a ruptured ACL ligament of the knee with a portion of the quadriceps tendon obtained from the leg.
A 20-year-old patient male visits the office, with the complaints of having a right knee problem. The patient was playing soccer and his cleats got stuck on the turf and his leg twisted.
The patient reports standing, walking, twisting, exercise, upstairs, and downstairs for aggravating factors with associated symptoms of swelling, instability, and pain with motion. Because of the different symptoms that the patient encountered, we agreed to go with 3 tesla MRI of Right knee.
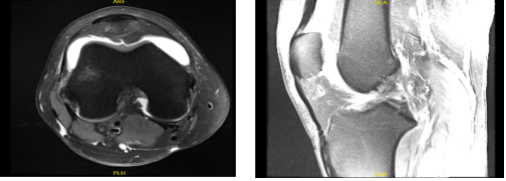
MRI results were presented and reviewed by the doctor, the result was discussed, the Ligaments are a full-thickness ACL tear with progression since the prior study. No posterolateral corner injury. The PCL, MCL and lateral collateral ligament complex and the extensor mechanism are Intact.
The lateral compartment is the complex tearing of the lateral meniscus posterior horn and horizontal tear of the anterior horn. There is partial-thickness cartilage loss and deep chondral fissuring along the central weight bearing aspect of the lateral femoral condyle with adjacent marrow edema indicative of bone contusions versus stress reaction.
There is mild partial-thickness cartilage loss along the posterior aspect of the lateral tibial plateau. The Medial Compartment is a longitudinal peripheral tearing of the medial meniscus at the posterior meniscocapsular junction on series 5 images 27-32.
There is focal full-thickness chondral fissuring along the inner aspect of the medial femoral condyle with faint stress reaction adjacent to the fissure. The patellar and trochlear cartilage are preserved.
The Tibial and femoral bone contusion pattern indicative of a recent anterior tibial translation. There is a large joint effusion. Muscles/Tendons are Intact, while the Neurovascular Structures and Subcutaneous Tissues are Unremarkable.
It has full-thickness ACL tear with bone contusion pattern indicative of a recent anterior tibial translation. The ACL tear has now progressed to full-thickness and is worse compared to the prior study.
The tearing of the medial and lateral meniscus, progressive in severity since the prior study. And slight partial-thickness cartilage loss and fissuring as discussed above. It also has large joint effusion, increased in size.
MRI-3T Right knee non-contrast
We discussed the treatment options for the patient’s diagnosis, which included living with the extremity as it is, organized exercises, medicines, injections and surgical options. We also discussed the nature and purpose of the treatment options along with the expected risks and benefits.
Also, we explained that there is no guarantee that all the function and strength will return. We have discussed the surgical procedure as well as the realistic expectations regarding the risks, outcome and post operative protocol. The patient has understood and expressed a desire to proceed with the surgery and signed an informed consent.
The patient was taken to the operating room and he was placed on a well-padded operating table. General anesthesia was induced. The right lower extremity was prepped and draped aseptically after application of tourniquet. Preop antibiotic was given. Time-out was called.
Tourniquet was not inflated at this time. Quadriceps tendon graft harvest was planned. A suprapatellar midline incision was given about 3 cm. With sharp dissection, the quadriceps tendon was reached.
With blunt dissection, the quadriceps tendon would be dissected proximally along the lateral border of vastus medialis obliquus. It was checked and removed with the arthroscope.
A 7 mm deep and 10 mm wide Arthrex preloaded blade was used to cut the graft, and was partially cut into the quadriceps tendon. The tendon has sharp dissection from over the superior port of the patella. Suture was passed into the distal quadriceps to have elevated.
With sharp dissection, a partial-thickness quadriceps graft was elevated for about 80 mm. There was a rent in the capsule, which was sealed later on with #0 Vicryl. The graft cutter was used to elevate the graft up to 80 mm and cut. The graft was removed and sutured.
The suprapatellar incision was packed with the Ray-Tec. Now, the tourniquet was elevated after the application of Esmarch. Arthroscope was entered through the lateral entry portal.
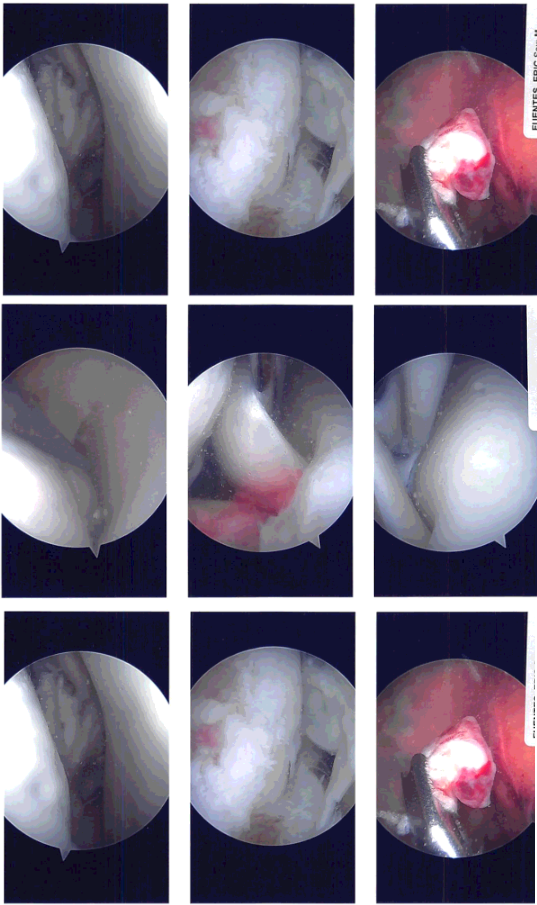
Examination of the patellofemoral compartment showed no arthritic changes. Examination of the medial patellofemoral compartment showed grade 3 to grade 4 change in a small patch over the medial femoral condyle.
The meniscus showed an inferior flap over the posterior horn, which was removed with the shaver. There was no ramp lesion or meniscal tear. The scope was entered into the Intercondylar notch where the ACL was found to be torn. The ACL was debrided with the use of a shaver. The PCL was intact.
The medial wall of the lateral femoral condyle was cleaned and debrided for identification of the footprint of the ACL. The tibial footprint of the ACL was also debrided. The arthroscope was entered into the lateral femoral condyle and lateral tibiofemoral compartment.
It showed grade 3 to grade 4 arthritic changes over a third of the femoral condyle. Also, there was a bad tear in the lateral meniscus, which was extending from the mid body to the posterior body and the posterior Hom across the popliteal hiatus.
Intraoperative Arthroscopy Images
After two weeks the patient is seen in the office for follow up checkup. The patient is doing well after the surgery. The has no other signs and symptoms and we decided to discuss the treatment options.
We will proceed with the formal physical therapy as well as a home exercise program for rehabilitation of the knee. We removed the stitches during today’s visit. We will continue with ice and elevation of the knee to decrease swelling and pain.
We will continue to utilize early mobilization and mechanical prophylaxis to reduce the chances of a deep vein thrombosis. We will wean them off any narcotic medications and progress to anti-inflammatories and Tylenol as long as there are no contraindications to these medications.
With the continued follow up checkup the patient showed progress from time to time he visits the office. He gets well after the surgery and with the help of continuing physical therapy.
Disclaimer – Patient’s name, age, sex, dates, events have been changed or modified to protect patient privacy.
I am Vedant Vaksha, Fellowship trained Spine, Sports and Arthroscopic Surgeon at Complete Orthopedics. I take care of patients with ailments of the neck, back, shoulder, knee, elbow and ankle. I personally approve this content and have written most of it myself.
Please take a look at my profile page and don't hesitate to come in and talk.