Case Study: Medial Meniscus repair performed
for Meniscal Cyst found from a 32 year-old male patient
The patient is being seen because of left knee pain. He has no recollection of any knee injuries. He had two instances of buckling about six weeks ago. He is in excruciating agony all of the time. He’s been hobbling for the past six weeks.
When he collapsed, he heard a crunch. There is no precedent of locking. Stains, deep knee bends, and position changes aggravate the discomfort. It is linked to edema. He has no previous medical background and no allergies. He does not take any pain relievers.
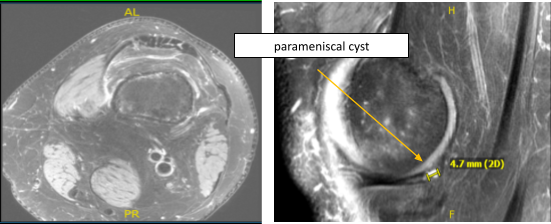
MRI was presented and shown An MRI was provided, which revealed a mild sprain of the medial collateral ligament but no tears. A 0.5 cm para meniscal cyst is linked with a longitudinal vertical tear affecting the outer third of the body and the posterior horn medial meniscus. There was mild fraying of the free border of the lateral meniscus. There was a tiny joint effusion and a lymph node in the popliteal fossae with an unknown etiology.
Upon examination of the left knee, the patient is tender to palpation along the medial joint line, and has an effusion. They are tender to palpation along the medial and lateral facets of the patella. They have crepitus of the patellofemoral joint with range of motion and discomfort with patella grind testing.
The patient has discomfort with McMurray’s maneuvers, and the knee is stable. They have limited range of motion. They have 5/5 strength, and are neurovascularly intact distally. There is no erythema, warmth or skin lesions present. On examination of the contralateral extremity, the patient is nontender to palpation and has excellent range of motion, stability and strength.
We attempted traditional physical therapy treatment for three months with no success. His discomfort has been getting worse. He also received a cortisone shot, which did not assist at all. He is in excruciating agony all of the time.
He’s been stumbling. Stairs, deep knee bends, and position changes aggravate the discomfort. It is linked to edema. He has no previous medical background and no allergies. He has been using a hinged knee support, but it has not been very effective.
The patient expressed a desire to continue with surgery, and I educated the patient on the inherent and unavoidable risks, which included, but were not limited to: anesthesia, infection, nerve and blood vessel damage, blood loss, blood clots, and even death.
We also discussed the chance of being unable to resume previous activities or employment, the need for future surgery, and complex regional pain syndrome. The patient is also aware that a lengthy rehabilitative process usually follows the surgical treatment.
I also stated that there is no assurance that all function and strength will be restored. The patient also understands the risks of re-tear or failure to heal. The patient expressed understanding of these risks and has elected to proceed with surgery.
Anesthesia was administered. After applying a mid-thigh tourniquet and using chlorhexidine paint, the left lower limb was prepared. A lateral working portal was established over the left knee. The scope was entered and examination of the knee was performed.
There was patellofemoral arthritis on the medial side of the patella. There was OA grade 1 to 2 patellofemoral arthritis on the medial facet of the patella and OA grade 1 to 2 arthritis of the medial femoral condyle.
Tear in medial meniscus involving the posterior horn were repaired. The repair of the bucket-handle tear stabled by Fast-Fix. During and final pictures were taken during the operation.
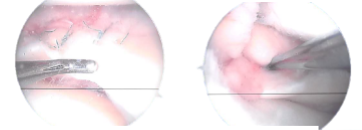
Final pictures showing operative part dressed
The knee was completely irrigated and shed. The knee was closed with nylon #3-0 sutures. Dry treatment was done with Adaptic, 4 x 4, and Webril and Ace Wrap. The ligature was taken off. The patient was successfully extubated.
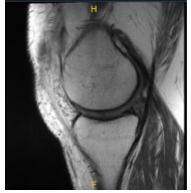
MRI presented to post operative visit, no visibility of the cyst
After a week, the patient showed signs of improvement in terms of discomfort and swelling. He walks with a limp and uses aids to get around. Denies having a temperature, chills, or reinjury. The incisions are healing well two weeks after operation, with no signs of drainage, erythema, or warmth.
There is a complete range of motion without pain. In order to rehab the knee, we have chosen to combine formal physical therapy with a home exercise regimen. Every 3-4 weeks, the patient returned to the office. The patient recovered well from the surgery and continued physical rehabilitation.
Disclaimer – Patient’s name, age, sex, dates, events have been changed or modified to protect patient privacy.
I am Vedant Vaksha, Fellowship trained Spine, Sports and Arthroscopic Surgeon at Complete Orthopedics. I take care of patients with ailments of the neck, back, shoulder, knee, elbow and ankle. I personally approve this content and have written most of it myself.
Please take a look at my profile page and don't hesitate to come in and talk.

