Case Study: Total Hip Replacement in a 65-year-old Male
with Avascular Necrosis of the Left Hip
A 65-year-old male presented to our office with complaints of left hip pain. The pain began 8 years ago but the patient didn’t recall any specific onset. Since the onset, the pain has worsened and the patient finds it difficult to walk and get up from sitting position. He reported consulting various doctors who told him that he has avascular necrosis. He was looking for surgical options for his hip pain.
The pain was described as moderate to severe in intensity located over the left groin which was constant. There was radiation to the left knee on activities such as walking and climbing stairs. The pain was described as a dull ache that would change to sharp on exacerbating activities. Recently he found it difficult to even tie his shoelaces. His current walking tolerance was less than a block.
The patient has previously tried treatment in the form of hip cortisone injections, NSAIDs, and physical therapy but with minimal relief. He was unable to squat and sit cross-legged. The patient was working as an accountant and his work involved frequent traveling, walking, climbing stairs and sitting for prolonged periods of time. The patient was unable to sleep comfortably at night.
He expressed dismay at his inability to work efficiently and being unable to do his daily activities. He was a past smoker (10 pack-years) and a social drinker. He denied any known drug allergies. His medical history included high blood pressure well-controlled with medications (amlodipine 10 mg). He previously had a cholecystectomy done 15 years ago. He denied any past history of trauma or surgeries around the hip.
The patient was using a cane for ambulation. His gait was antalgic with a reduced stance phase on the left side. Bilateral shoulders, anterior and posterior iliac spines, patella, and medial malleolus were at the same level. There was no evidence of scoliosis and exaggerated lumbar lordosis.
The skin overlying the left hip was normal with no scars or sinus tracts. On palpitation, there was left anterior hip joint line tenderness. There was no fullness or swelling in the left groin. There were no enlarged inguinal lymph nodes. The power and bulk of bilateral lower extremity muscles were intact.
The range of motion was not restricted but painful in internal rotation and abduction. There was no leg length discrepancy and no fixed deformities. The examination of the right hip revealed tenderness at the right greater trochanter suggesting bursitis. The examination of bilateral knees and ankles were normal.
There was no distal neurological deficit and power sensory examination of lower extremities was normal. There was no abnormality of the bladder, bowel function.
Imaging revealed osteoarthritic changes of the left hip with an AVN lesion that involves 60% of the femoral head. An MRI was obtained which revealed left femoral head avascular necrosis without overt subchondral collapse.

X-ray showing the AP view of the pelvis with both hip joints.
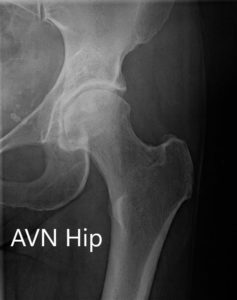

X-ray showing the AP and frog-legged lateral views of the left hip joint.
Considering the patient’s condition, and having exhausted conservative management, he was offered a left total hip replacement. Risks, benefits, and alternatives were discussed with the patient and his family at length. He agreed to go ahead with the surgery.
Operation: Left total hip arthroplasty.
Implant used: Acetabular shell 60 mm with a 6.5 mm x 30 mm cancellous screw, with ceramic femoral head 36 mm, 0-degree polyethylene with 127-degree neck angle hip stem.
Description of the procedure: The patient was brought to the operating room after obtaining informed consent and signing the correct surgical site. The risks, benefits, and alternatives were extensively discussed with the patient prior to the procedure. The patient was brought to the operating room and anesthesia was obtained by the anesthesiologist.
The patient was definitively positioned with the left hip up and the left hip was then draped and prepped in the usual sterile manner. The straight incision centered over the greater trochanter was used for the arthrotomy. Skin and subcutaneous tissues were then incised. The fascia was then divided.
The acetabulum was then exposed. The remainder of the labrum was then debrided. The acetabulum was reamed and the final shell was then placed into position in the correct abduction and anteversion.
The shell was then placed over the cup after the placement of the screw. Attention was then turned towards the femur. The remainder of the tissue on the undersurface of the greater trochanter was then removed. The femur was then sequentially broached and the final broach was left into position.
The trunnion was then placed over the shell and the head was then placed over the trunnion. The pre-robotic plan was used in the assessment of the height. The lesser trochanter to center distance was also measured preoperatively before making the neck resection and was also compared after placement of the trial component. The hip was then reduced and trialed through a full range of motion and the hip was stable in all physiological range of motion.
The hip was dislocated. Trial components were then removed. The final components were then placed into position. The hip was then reduced again. A thorough lavage was given. The posterior soft tissue structures were then tacked to the greater trochanter through transosseous tunnels. Thorough lavage was given.
The fascia was closed, cutaneous tissues were closed, subcutaneous tissues were closed. The skin was closed using staples. Sterile dressing was then applied over the wound and the patient was then transferred to the postoperative care unit in stable condition.

Postoperative X-ray of the pelvis showing AP and lateral views.
The pathology report from the excised femoral head suggested degenerative disease with bone and marrow necrosis.
The recovery of the patient was excellent. The pain was managed with oxycodone and acetaminophen. An abduction pillow was used and hip precautions were explained to the patient. Aspirin 325mg BID was started for DVT (Deep vein thrombosis) prophylaxis. Sutures were removed on post-op day 14 uneventfully. There was no distal neurological deficit.
Home exercise program and physical therapy were initiated for gait training, fall prevention, strengthening age increasing range of motion. Weight-bearing was allowed as tolerated. After three months, the patient was back to his baseline activity. He had some returned to work and was very happy with the outcome.
Disclaimer – Patient’s name, age, sex, dates, events have been changed or modified to protect patient privacy.

Dr. Suhirad Khokhar
My name is Dr. Suhirad Khokhar, and am an orthopaedic surgeon. I completed my MBBS (Bachelor of Medicine & Bachelor of Surgery) at Govt. Medical College, Patiala, India.
I specialize in musculoskeletal disorders and their management, and have personally approved of and written this content.
My profile page has all of my educational information, work experience, and all the pages on this site that I've contributed to.
