Case Study: Knee Arthroscopy: ACL Repair using Fiber Link
Internal Brace and Tight Rope with Distal Fixation using
SwiveLock and Chondroplasty in a 51 year-old female
In general, three transplant alternatives are available: a patellar tendon autograft, a hamstring autograft, and an allograft. In this case, surgeons anatomically narrow the space, drill across the two bones, and implant a hefty non-absorbable suture construct with metallic buttons at either end (the “tightrope”) to keep the bones together.
After repair, the internal brace functions as a secondary stabilizer, allowing for quicker rehabilitation and return to sports while resisting injury recurrence when possible.
A 51 year-old female patient visits the office with complaints of right shoulder and right knee pain for about months. She had pain and swelling in the left knee along with buckling and instability. Patient is allergic to penicillin and latex. MRI showed a tear of the proximal ACL.
Osseous structures: Alignment of the thoracic spine is anatomic. There are no compression deformities. The bone marrow signal is overall age-appropriate. Paraspinal soft tissues: The visualized paraspinal soft tissues are grossly unremarkable.
Intervertebral discs: A left paramedian disc herniations present at T6-T7 level impinging on exiting left C7 nerve roots, causing mild spinal canal stenosis. No spinal canal stenosis is present. The neural foramina are patented.
Spinal cord: No areas of focal signal abnormality are present in the thoracic spinal cord. The conus medullaris terminates at the T12 level and is within normal limits. The left paramedian disc herniation at T6-T7 level causes mild mass effect on the existing left C7 nerve roots.
The collateral ligaments has edema surrounding the medial collateral ligament compatible with a grade 1 partial tear. The lateral collateral ligament, biceps femoris tendon, iliotibial band, and popliteus tendon is intact. The cruciate ligaments is a full-thickness tear of anterior cruciate ligament proximally.
Posterior cruciate ligament is intact. The Menisci, the lateral and medial meniscus are intact. Cartilage, the chondral surfaces in the medial compartment and lateral compartment are intact also the anterior compartment is intact.
In bones, there is bone marrow edema in the posterior lateral tibial plateau compatible with micro trabecular fracture. Extensor Mechanism, there is a moderate to large knee joint effusion. No joint effusion and popliteal cyst are identified. The soft tissues are otherwise normal and the neurovascular structures demonstrate normal course.
It has an impression of complex tear of the anterior cruciate ligament proximally with associated likely trabecular fracture posterior lateral tibial plateau. Grade 1 partial tear in the medial collateral ligament. Moderate to large knee joint effusion.
We discussed treatment options and the patient opted for surgical management.
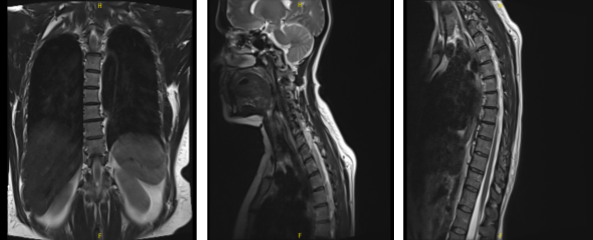
MRI-3T Thoracic Spine non-contrast
We discussed risks and benefits including infection, bleeding, injury to adjacent nerves and vessels, rehabilitation, knee stiffness, need for manipulation, failure and need for repeat surgery, possibility of doing a repair, which may fail and need for reconstruction, possibility of doing a reconstruction if the tear is not repairable, possibility of development of arthritis in future and need for total knee replacement among others.
We also discussed systemic complications including blood clots, cardiac, pulmonary, neurological complications including death. The patient understood and signed an informed consent.
The patient was taken to the operating room where she was placed on a well-padded operating table. General anesthesia was induced. IV clindamycin was given as a pre op antibiotic. Left lower extremity was prepped and draped aseptically in a usual fashion after application of high tourniquet.
The leg was held in a leg holder. Timeout was called. A tourniquet was applied and elevated at 325 mmHg. The 111 minutes of tourniquet time was used during the surgery.
Lateral entry portal was made and an arthroscope was entered. showed grade 2 to grade 3 patellar chondral lesions on the left facet. Examination of the medial tibiofemoral compartment showed intact medial meniscus and cartilage. The Medical entry portal was made using a spinal needle.
Probe was also used to examine the knee. Examination of the lateral tibiofemoral compartment showed intact meniscus and cartilage. Further examination of the intercondylar notch showed proximal tear of the ACL right from the bone.
There was minimal bone stump. Shaver was used to clear the fat pad of ACL from PCL as well as at its attachments.
The bone was debrided with a shaver. Decision was made to repair the ACL. Scope was entered into the patellofemoral joint where chondroplasty of the patella was performed using a shaver. Scope was brought back into the intercondylar notch. A Passport was inserted on the medial portal to allow access.
Scorpion was used to pass Fiberlink sutures x2, one each to the anteromedial and posterolateral bundle of ACL. The sutures were brought out through a secondary portal super medially. Now, the exit portal of the femoral condyle was marked and the canal was drilled using the ACL FlipCutter.
A 4-mm straight tip drill was tried to use through an accessory medial portal, but direction of the canal was too inferior. Finding an appropriate canal with the ACL Fiber Stick was passed the loop. Internal Brace Fiber Tape was loaded over a Tightrope RT.
One of the leading sutures was removed and one Fiber Link was passed through the hole and another Fiber Link was passed through the hole of the Tightrope.
These sutures were shuttled through the femoral tunnel and brought out. The button was brought out and flipped. Now, the passing suture from the Fiber Links were removed and ABS was tied while examining arthroscopically into the knee.
Once the Internal Brace was into the femoral tunnel, tibial tunnel was drilled using a tibial zig and Fiber Stick was again used to pass the loop. The distal end of the fiber Internal Brace was passed to the loop towards tibial tunnel. The Internal Brace was found to be in satisfactory position.
The distal tip of the tibial tunnel was tightened for SwiveLock #4.75 Arthrex. Now, the ABS was tightened proximally and tied over each other. The Fiber Links were also tightened and tied over each other.
Examination of the ACL with arthroscopy showed satisfactory direction to the bone. The Internal Brace was in satisfactory position. Final pictures were taken and saved.
The knee was copiously irrigated and drained. Closure was done using #2-0 Vicryl and #3-0 Nylon. 10 cc of Naropin was injected into the knee. Dressing was done using Xeroform, 4×4, ABD, Webril, Ace wrap. Knee immobilizer was applied in a -10-degree tension. The patient was extubated and moved to recovery in a stable condition.
The patient seen by the doctor or her one week post operative visit, no x-rays were needed. She denies fever, chills, and difficulty in pain are controlled. She stopped narcotics 2 days back.
After discussing treatment options, we have decided to proceed with formal physical therapy as well as a home exercise program for rehabilitation of the knee. We went over the arthroscopic pictures and removed the stitches during visits.
We will continue with ice and elevation of the knee to decrease swelling and pain. We will continue to utilize early mobilization and mechanical prophylaxis to reduce the chances of a deep vein thrombosis.
We will wean them off any narcotic medications and progress to anti-inflammatories and Tylenol as long as there are no contraindications to these medications. We also discussed the risk and benefits and common side effects of taking this medication. The patient will be back in three weeks’ time to evaluate their progress.
After 4 weeks the patient visits the office for her post operative consultation, she denies fever, chills, the pain has been improving, though slow. She has been working with PT and making slow progress. We agreed to go with conservative management for now.
We discussed goals and the need for more rigorous involvement. She is motivated but has a low threshold for pain which has made rehab difficult. She is trying her best. We encouraged her and discussed home therapy also.
The patient went to the office for her 8 week post operative visit, no x-rays were needed, she denies all symptoms of fever, chills, the pain has been improving, though slow. She has been working with PT and making progress; however, she has difficulty lifting her leg up in the air.
We advised her to use an ice machine and CPM. With the continued follow up checkup the patient showed progress from time to time she visits the office. She gets well after the surgery and with the help of continued physical therapy.
Disclaimer – Patient’s name, age, sex, dates, events have been changed or modified to protect patient privacy.

Dr. Vedant Vaksha
I am Vedant Vaksha, Fellowship trained Spine, Sports and Arthroscopic Surgeon at Complete Orthopedics. I take care of patients with ailments of the neck, back, shoulder, knee, elbow and ankle. I personally approve this content and have written most of it myself.
Please take a look at my profile page and don't hesitate to come in and talk.
