Case Study: Medial and Lateral Meniscectomy
and Chondroplasty in a 59-year-old female
The medial meniscus and lateral meniscus serve as a shock absorber, and which helps to keep the knees steady and functional. Their appearance are crescent-shaped bands of thick, rubbery cartilage glued to the tibia.
Performing a surgery will help to prevent severe injury on the meniscus. Since having meniscus tear is a serious case, this can lead you to have long-continuing knee problems, such as arthritis. Moreover, breakage in the cartilage into the joint may result in considerable knee problems due to having a torn meniscus.
A 59-year-old patient was in our office, with complaints of right knee pain. Patient started her daughter’s dog, ran into her by accident and made her knee bend the wrong way. She said that her right knee makes clicking noises and the pain starts in the back of the knee and her sciatica hurts as well.
The pain is extremely severe in intensity, she described the pain as sharp, dull, stabbing, throbbing, aching, burning. The pain is constant and does disturb sleeping. The pain is associated with bruising but not with swelling, tingling, numbness, radiating pain, weakness, bowel or bladder abnormality, gait problem, giving way, or limping, hand function difficulty. Walking, standing, and bending make the symptoms worse.
But rest and heat make the symptoms better. The patient has undergone surgery for back, lung, colon, fluoroscopic surgery, heel spurs, and carpel tunnel. Patient has fibromyalgia, lyme disease, and arthritis. Patient has palpitations to epinephrine. Patient is currently taking pain medication. Patient is a smoker.
Upon examination of the right knee, the patient is tender to palpation along the lateral joint line and has an effusion. Patient also has PF crepitus and tenderness on palpation along the medial and lateral PF joint line. Patellar grinding test is positive.
The patient has discomfort with McMurray’s maneuvers, and the knee is stable. They lack full flexion secondary to the effusion but have full extension. They have 5/5 strength and are neurovascularly intact distally.
There are no erythema, warmth or skin lesions present. On examination of the contralateral extremity, the patient is nontender to palpation and has excellent range of motion, stability, and strength. There are no fractures in the right knee, according to the X-ray results, which showed a normal right knee.
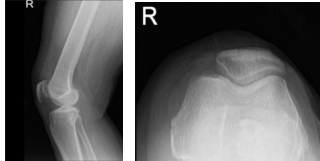
Right Knee X-ray AP and Lateral
MRI results showed moderate popliteal cyst. Mild lateral patellar subluxation. Medial meniscus tear, new compared to the August 2016 MR study. Chondromalacia as detailed below. Subchondral marrow signal changes associated with patellar chondromalacia have resolved since the previous study.
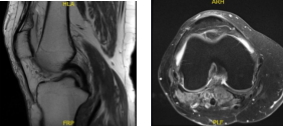
MRI – 3T Right Knee Non-Contrast
We discussed the treatment options for the patient’s diagnosis, which included living with the extremity as it is, organized exercises, medicines, injections, and surgical options. We also discussed the nature and purpose of the treatment options along with the expected risks and benefits.
I educated the patient regarding the inherent and unavoidable risks which include, but are not limited to anesthesia, infection, damage to nerves and blood vessels, blood loss, blood clots, and even death were discussed at length.
The patient also understands there is a long rehabilitative process that typically follows the surgical procedure and the possibility of not being able to return to prior activities or employment, the need for future surgery, and complex regional pain syndrome.
The patient also understands the risks of re-tear or failure to heal. The patient understands implants may be utilized during this surgery, also explained there is no guarantee all the function and strength will return.
The patient expressed understanding of these risks and has elected to proceed with surgery. We have discussed the surgical procedure as well as the realistic expectations regarding the risks, outcome and post operative protocol.
The patient was taken to the operating room where she was placed on a well-padded operating table. General anesthesia was induced. Low tourniquet was applied. IV antibiotics were given, before the tourniquet. A lateral entry portal was made. Arthroscope was entered into the patellofemoral joint and then into the medial compartment.
Then, the arthroscope was moved to the lateral compartment where a tear was seen. A medial entry portal was made with direct access to the left meniscus. The instruments were entered and the lateral margin of the medial meniscus, the fraying on the lateral margin of the medial meniscus was cleaned using a shaver.
The arthroscope was entered into the intercondylar area where there was partial tearing of the ACL fibers. The arthroscope was entered into the lateral femoral compartment where the tear was again seen. The third tear was thoroughly debrided using a shaver and straight bitter.
After the thorough debridement of the tear, the scope was moved into a patellofemoral joint where grade 3 to grade 4 osteoarthritic changes were seen. Chondroplasty of the posterior patellar surface was performed using a shaver.
There was grade 1 osteoarthritic change in the trochlea. was grade 1 to 2 osteoarthritic changes in the medial femoral compartment, medial femoral condyle posteriorly, which was shaved.
Now, the arthroscope was entered into the medial working portal and instruments were entered from the lateral portal. Final debridement of the lateral meniscus was performed. The knee was thoroughly irrigated and lavaged.
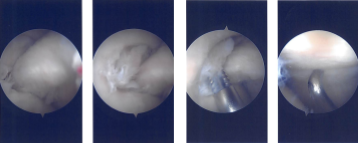
Intraoperative Arthroscopy Images
Final pictures were taken and saved. The scope was removed, and the knee was closed using #3-0 nylon. The 80 mg of Depo-Medrol and 18 mL of 0.5% Naropin was injected into the knee.
Dressing was performed using Adaptic, 4x4s, Webril and Ace wrap. The tourniquet was deflated and removed. The patient was extubated and moved to recovery in a stable condition.
The patient was seen for post operative check up. We have decided to do formal physical therapy as well as a home exercise program for rehabilitation of the knee. The patient regularly followed an office visit every 3-4 weeks.
Patient did well after the surgery and continued physical therapy. Patient checked in for a follow up visit after a month and saw significant improvement on her knee.
Disclaimer – Patient’s name, age, sex, dates, events have been changed or modified to protect patient privacy.

Dr. Vedant Vaksha
I am Vedant Vaksha, Fellowship trained Spine, Sports and Arthroscopic Surgeon at Complete Orthopedics. I take care of patients with ailments of the neck, back, shoulder, knee, elbow and ankle. I personally approve this content and have written most of it myself.
Please take a look at my profile page and don't hesitate to come in and talk.
