Case Study: Knee Arthroscopy: Medial and Lateral
Meniscectomy with Chondroplasty Microfracture and
Debridement of ACL in a 34 year-old male
The shinbone (tibia) is covered in thick, springy bands of cartilage called the medial and lateral meniscectomy. Meniscectomy, which involves removing the torn portion of the meniscus, is one fundamental method for treating a torn meniscus.
Another method involves sewing the torn portions of the meniscus back together. To try to minimize roughness, the articular cartilage is typically merely polished (“chondroplasty”).
A procedure known as microfracture can be used to cure some portions of articular cartilage that have peeled off down to bare bone. An arthroscope is used during the surgical operation known as debridement or a clean-up.
During this operation, surgical instruments are used to remove the damaged cartilage or bone, and the rough edges of the articular cartilage will be smoothed down.
The patient is a 34 year-old male seen in the office multiple times in the past. He has had pain in the right knee on the inner side, which has not been relieved with nonoperative treatment in the form of physical therapy, chiropractics, and antiinflammatory medications. MRI was done.
MRI were reviewed and discussed; the Linear signal elevation is identified within the posterior hom of the medial meniscus on coronal sequence image #12 and sagittal sequence image #26 associated with intrasubstance tears. Tear within the lateral meniscus is not appreciated.
Preservation of joint space height is noted in both medial and lateral femorotibial compartments. Intermediate signal intensity is noted in association with the anterior cruciate ligament suggestive of sprain.
There is no evidence of discontinuity or retraction of the posterior cruciate ligament to indicate tear. There is no evidence of tear of the medial collateral ligament. There is no evidence of tearing of the lateral collateral ligament.
There is no evidence of tearing of the quadriceps tendon. There is no evidence of tearing of the patellar tendon. There is no evidence of tear of the medial or lateral patellar retinaculum. Popliteus peritendinous fluid associated with tenosynovitis.
Semimembranosus and semitendinosus peritendinous fluid is also associated with tenosynovitis. There is no evidence of signal changes associated with the iliotibial band. There is no evidence of degenerative changes of the proximal tibiofemoral articulation.
Mild joint effusion is noted with both suprapatellar and infrapatellar components. There is no evidence of Baker’s cyst posterior to the medial femoral condyle. There is no evidence of chondromalacia within the posterior patella.
Tibial tubercle to trochlear groove distance measures approximately 5 mm within normal limits. Trace anterior soft tissue edema is noted. There is no evidence of bone marrow signal change to indicate fracture, avascular necrosis, osteomyelitis or bone marrow replacement process.
Impression: Intrasubstance tear posterior horn of the medial meniscus. Anterior cruciate ligament sprain. Popliteus, semimembranosus, and semitendinosus tenosynovitis and mild effusion. Which means that the MRI results showed medial meniscus tear and tearing of the ACL.
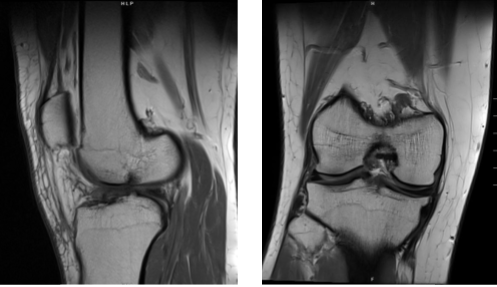
Magnetic resonance imaging scan of the right knee
We discussed the treatment options and the patient opted for surgical management. We discussed risks and benefits including infection, bleeding, injury to adjacent nerves and vessels, inability to heal and need for repeat surgery, need for rehabilitation, knee arthritis, knee stiffness among others.
We also discussed systemic complications including blood clots, cardiac, pulmonary, neurological complications including death. The patient understood and signed an informed consent.
The patient also had issues with managing his potassium levels and he had been on oral potassium for some time. He was asked to continue seeing his primary care doctor for the same.
The patient was taken to the operating room where general anesthesia was induced. Right lower extremity was prepped and draped aseptically in the usual fashion. Time-out was called. Preop antibiotic was given.
An Esmarch was applied and tourniquet elevated at 300 mmHg. Lateral entry portal was made through a parapatellar incision. Arthroscope was inserted. A medical entry portal was made with the use of a spinal needle.
Examination of the patellofemoral joint showed intact cartilage of the patella. Examination of the medial compartment showed grade 1 osteoarthritic changes of the medial femoral condyle plus a lesion of the medial meniscus along the body in the posterior horn at the red-red zone junction in the form of capsular separation. A decision was made to repair the meniscus.
Examination of the intercondylar notch showed partial tearing and fraying of the ACL. Debridement of the ACL was done. Partial continuity ACL was present and decision was made not to repair the ACL at present and will be dealt with rehabilitation.
Examination of the lateral compartment showed fraying and tearing of the medial margin of the lateral meniscus. Biters and shavers were used to complete the lateral meniscectomy. Now, the arthroscope was inserted from the medial portal and findings were verified.
Fast-Fix was used to repair the medial meniscus. The skin was entered from the medial side and two reverse FasT-Fix and one curved FasT-Fix were used to repair the medial meniscus with horizontal mattress sutures x3.
Rasp was used before application of the sutures to prepare the site. Spinal needle was used to pie-crust to MCL to achieve more space in the medial femoral compartment.
Also, the spinal needle was used to perform fenestration of the capsule as well as the meniscus. Fast-Fix was used x3 and good apposition and reduction of the meniscus was achieved.
Final pictures were taken and saved. Microfracture was performed at the intercondylar notch of the right knee with the condylar defect. could be seen coming out of this microfracture. The knee was thoroughly irrigated. Final pictures were taken and saved.
The knee was drained and closure was done with the use of # 3-0 nylon. Then 20 cc of 0.5% Marcaine was injected into the knee. The patient was extubated. The dressing was done with the use of Xeroform, 4x8s, ABD, Webril, and Ace wrap. Knee immobilizer was put in to keep the knee in extension.
After one week the patient was seen in the office for his postoperative visit, no x-rays were needed. The patient presents with left shoulder and right knee pain along with low back pain due to a MVA a few months ago.
He Had no pain before that happened, his left shoulder pain has been improved but his right knee pain is still bothering him. After discussing treatment options, we have decided to proceed with formal physical therapy as well as a home exercise program for rehabilitation of the knee.
We went over the arthroscopic pictures and removed the stitches during the visit. We will continue with ice and elevation of the knee to decrease swelling and pain. We will continue to utilize early mobilization and mechanical prophylaxis to reduce the chances of a deep vein thrombosis.
We will wean them off any narcotic medications and progress to anti-inflammatories and Tylenol as long as there are no contraindications to these medications.
We also discussed the risk and benefits and common side effects of taking these medications at today’s visit. I will see them back in three weeks’ time to evaluate the progress.
After one month the patient went to the office for his post operative visits, no x-rays needed. He has some pain on the inner knee. He is using crutches and braces. We discussed treatment options including PT, MRI, Injection, surgery and we agreed to go with conservative management for now.
Like, he is about to work with his Physical therapy, Ice/heat, Elevation and OTC anti-inflammatory meds to control pain and swelling. Follow up checkup after 4 weeks.
After two months the patient visits the office for his postoperative consultations, he has been working with PT and has no pain in the knee however, he is still using braces.
With the continued physical therapy and rehabilitation of the knee, the patient did well after the surgery, from the time of his visits he is gradually improving. Through regular visits and continued physical therapy, the patient healed and recovered.
Disclaimer – Patient’s name, age, sex, dates, events have been changed or modified to protect patient privacy

Dr. Vedant Vaksha
I am Vedant Vaksha, Fellowship trained Spine, Sports and Arthroscopic Surgeon at Complete Orthopedics. I take care of patients with ailments of the neck, back, shoulder, knee, elbow and ankle. I personally approve this content and have written most of it myself.
Please take a look at my profile page and don't hesitate to come in and talk.
