Case Study: Management of Adhesive Capsulitis
of the Left Shoulder in a 55-year-old Male
The patient is a 55-year-old male being seen today with complaints of the left shoulder pain due to a motor vehicle accident that occurred a year ago. He had left shoulder arthroscopy done by an outside physician last year. Acromioplasty and subacromial debridement were performed. Following the surgery, the patient started developing adhesive capsulitis, which was being treated conservatively with physical therapy.
The shoulder pain is associated with restriction of movement and is sharp at times. It is aggravated by sudden movements. The patient is left-handed and he finds it extremely difficult to perform daily activities such as combing hair, lifting things, driving, playing with his grandkids, and maintaining personal hygiene.
The patient had been recovering well with therapy. Recently, the patient had an abdominal surgery following which the left shoulder movements deteriorated. The patient works as a medical receptionist at a medical office.
The patient is a nonsmoker and social drinker. He denies any known drug allergies. His medical history included hypertension, asthma, and hyperlipidemia. All his medical conditions are under control with medications.
On examination, the patient is calm, conscious cooperative, and well oriented to time place and person. Upon examination of the left shoulder, the patient sits with the scapula protracted and depressed. There is tenderness to palpation over the trapezius and rhomboids as well as the anterior aspect of the supraspinatus and biceps.
There is no tenderness to palpation over the neck, clavicle, scapula, and elbow. There is no soft tissue swelling and ecchymosis. The patient has a limited range of motion of the shoulder in all planes secondary to discomfort (40 abduction, 30 external rotation, Internal rotation till SI).
The patient is unable to tolerate stability testing. Strength in rotator cuff muscles in 4+/5 and associated with pain. Hawkins’s test is positive, Neer’s test is negative. Distal neurovascular is intact.
On examination of the contralateral extremity, the patient is nontender to palpation and has an excellent range of motion, stability, and strength.
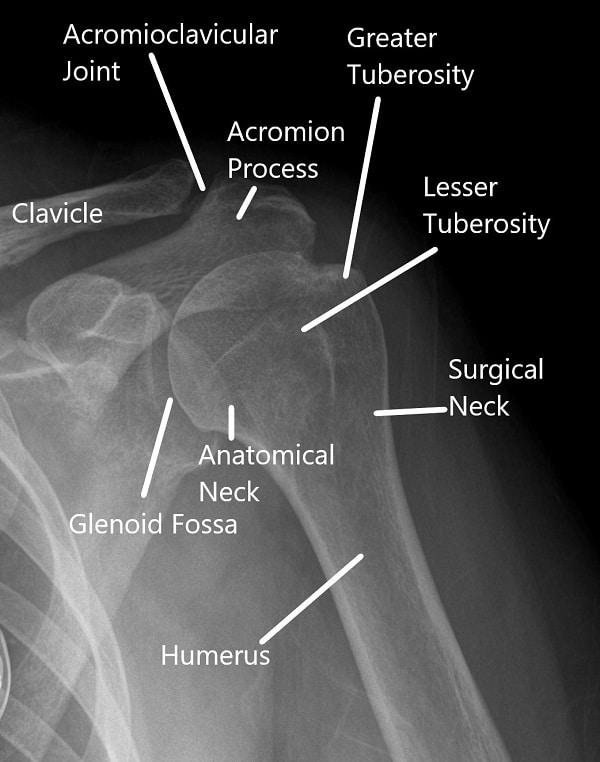
X-ray of the shoulder in AP view
MRI of the left shoulder suggested tendinosis of the supraspinatus tendon with a partial articular surface tear of the anterior and mid substance fibers of the tendon. Tendinosis of the infraspinatus tendon. Subacromial/subdeltoid bursal fluid reflecting bursitis. Degeneration and tear of the anterosuperior labrum.
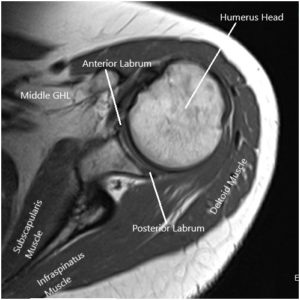
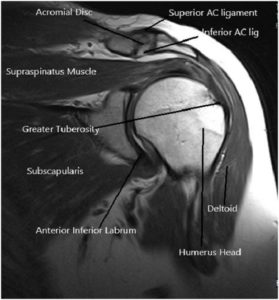
MRI image of the shoulder in axial and coronal sections
We discussed treatment options and the patient opted for surgical management in the form of manipulation under anesthesia. We discussed risks and complications of the surgery including fracture, re-recurrence of adhesive capsulitis, inability to regain full range of motion, need for arthroscopic capsular release, swelling, pain, rehabilitation amongst others. The patient understood the risks and benefits and complications and signed informed consent.
PREOPERATIVE DIAGNOSIS: Adhesive capsulitis of the left shoulder.
POSTOPERATIVE DIAGNOSIS: Adhesive capsulitis of the left shoulder.
OPERATION: Manipulation under anesthesia followed by cortisone injection in the left glenohumeral joint.
DESCRIPTION OF PROCEDURE: The patient was taken to the operating room where she was kept on the transport stretcher herself. The patient was given a brachial block before entering the room by the anesthesiologist.
Conscious sedation was done and once the patient was fully sedated, the left shoulder was manipulated under anesthesia. Crepitus of rupture of the adhesions would be felt while doing the abduction and internal rotation. A complete range of motion was achieved under anesthesia.
Following that, 80 mg of Depo-Medrol mixed with 3 ccs of 0.5% Marcaine and 3 ccs of 1% lidocaine was injected in her left glenohumeral joint. The patient was moved to the postoperative stay unit in a stable condition.
Disclaimer – Patient’s name, age, sex, dates, events have been changed or modified to protect patient privacy.

Dr. Suhirad Khokhar
My name is Dr. Suhirad Khokhar, and am an orthopaedic surgeon. I completed my MBBS (Bachelor of Medicine & Bachelor of Surgery) at Govt. Medical College, Patiala, India.
I specialize in musculoskeletal disorders and their management, and have personally approved of and written this content.
My profile page has all of my educational information, work experience, and all the pages on this site that I've contributed to.
