Case Study: Right Knee Arthroscopic Lateral Release
in a 36-year-old patient
An arthroscopic procedure called lateral release surgery for the knee is carried out through three-minute incisions. In order to get the kneecap to slide perfectly into the right groove and return to its natural alignment, a medical professional will cut through a tight clump of tendons in the kneecap.
Injury to one or more of the ligaments, tendons, cartilage, bones, or muscles that make up the knee joint is referred to as a knee injury. These injuries can be brought on by falling, twisting the knee violently, heavy impact from a car accident, or other forces.
A 36-year-old patient was in our office with complaints of right and left knee pain. The patient remembers no injury. The pain is extremely severe in intensity. The patient describes the pain as sharp and constant but does not disturb sleep.
The pain is associated with swelling, weakness but is not associated with bruising, numbness, tingling, radiating pain, bowel or bladder abnormality, gait problem, or limping, giving way, and hand function difficulty. Walking, standing, lifting, twisting, lying in bed, bending stairs, sitting make the symptoms worse. Medication makes the symptoms better.
The patient has had back fusion surgery in the past. Her back still bothers her along with bilateral radiculopathy occasionally. Patient does not smoke or use recreational drugs. The patient is not allergic to any drug.
X-ray results showed that there are no significant degenerative changes and there are no fractures. The patient was advised to take an MRI in order to show the reason which caused pain in her knee.
The patient’s MRI results showed minimal chondral wear over the patella and lateral tibial plateau. No evidence of meniscal tears. Mild patellar tendinosis.

Right Knee X-ray
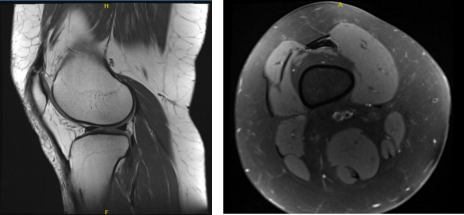
MRI Right Knee Non-contrast
We discussed the treatment options for the patient’s diagnosis, which included living with the extremity as it is, organized exercises, medicines, injections, and surgical options. We also discussed the nature and purpose of the treatment options along with the expected risks and benefits.
I educated the patient regarding the inherent and unavoidable risks which include, but are not limited to anesthesia, infection, damage to nerves and blood vessels, blood loss, blood clots, and even death were discussed at length.
We also talked about the possibility of not being able to return to prior activities or employment, the need for future surgery, and complex regional pain syndrome.
We talked about the possibility of not being able to alleviate all the discomfort. Also, I explained there is no guarantee all the function and strength will return. The patient also understands the risks of re-tear or failure to heal. The patient understands implants may be utilized during this surgery.
The patient expressed understanding of these risks and has elected to proceed with surgery. We have discussed the surgical procedure as well as the realistic expectations regarding the risks, outcome, and post operative protocol.
The patient was taken to the operating room where she was placed on a well-padded operating room table. General anesthesia was Induced. The right lower extremity was prepped and draped aseptically in the usual fashion.
The left lower extremity was put on a well-padded pillow. Preoperative antibiotic was given. The tourniquet was inflated. Arthroscope was set up.
A lateral entry portal was made, and the arthroscope was introduced. Examination of the knee showed intact articular cartilage. A Medical entry portal was made.
Examination of the meniscus and ACL showed that they were intact. Patellar maltracking was checked and found that the patella was laterally set in the initial 30-degrees of motion.
On deep inspection, the patella was well set in the trochlea. A decision of lateral release was made. The scope was entered on the medial side. Blunt trocar was entered, and a tunnel was made lateral to the lateral capsule. The ablator was introduced, and lateral release was performed. Using the ablation, we achieved hemostasis.
The tourniquet was released. The motor supply was stopped to find any bleeders and hemostasis was achieved thoroughly. The knee was irrigated and draped. Closure was done using #3-0 nylon. Marcaine 9 cc and 1 cc of 40 mg of Depo-Medrol was injected into the knee.
Dressing was performed using 4×4, Webril, and Ace wrap. The knee immobilizer was applied. The patient was extubated and moved to recover in a stable condition. The patient was seen for a post operative check up.
We have decided to do formal physical therapy as well as a home exercise program for rehabilitation of the knee. The patient did well after the surgery and continued physical therapy. Patient checked in for a follow up visit after a month and saw significant improvement on his knee.
Disclaimer – Patient’s name, age, sex, dates, events have been changed or modified to protect patient privacy.

Dr. Vedant Vaksha
I am Vedant Vaksha, Fellowship trained Spine, Sports and Arthroscopic Surgeon at Complete Orthopedics. I take care of patients with ailments of the neck, back, shoulder, knee, elbow and ankle. I personally approve this content and have written most of it myself.
Please take a look at my profile page and don't hesitate to come in and talk.
