Case Study: Primary Total Hip Arthroplasty
in an 84-year-old female for Hip Arthritis
An 84-year-old female with multiple comorbidities presented to our office with complaints of worsening right hip pain. She was a retired accountant previously working at the World Trade Center 25 years ago. She was married living with her husband. She was active socially and regularly went to a book club interacting with readers and writers.
She first noticed the pain 2 years ago which had since worsened in intensity (7/10). The pain was located in the right groin described as a dull ache with no radiation. The pain was exacerbated on activities such as walking, climbing stairs and getting up from sitting position.
Recently the pain has been interfering with her daily activities. She reported the inability to put on her socks and shoes, doing her laundry and increasing stiffness after sitting for a long period. She had stopped her routine of going to the book club and felt stressed about it.
She had consulted outside physicians who diagnosed her with arthritis. She had since tried Hip injections and physical therapy but with limited relief. She started using a cane as a walking aid. Her husband accompanied her to the office visit and both expressed anguish at her reduced mobility and pain.
She had a medical history of atrial fibrillation, asthma, sleep apnea, low back pain, and hypertension. Her past surgical history included a hysterectomy 5 years ago and multiple caudal epidural injections for low back pain. She was on blood thinners in the form of Xarelto. Her other medications included Albuterol pump, Bystolic and Lopressor.
She was a nonsmoker with seasonal allergies and no known drug allergies. On her physical examination, her gait was antalgic with a reduced stance phase on the right side. There was leg length discrepancy and no exaggeration of lumbar lordosis.
There was absence of any fullness in the right Scarpa’s triangle. There was no lymphadenopathy and no superficial tenderness. Deep palpation revealed the right anterior joint line tenderness. There was an absence of any trochanteric tenderness.
The range of motion was restricted in abduction and external rotation with pain at end movements. The left hip, bilateral ankles, and knees were normal. There was no distal neurological deficit and bilateral lower extremity pulses were 2+ and palpable. She denied any long term steroid or alcohol abuse.
Radiographs of the pelvis revealed osteoarthritic changes in the right hip. Considering her comorbidities and lifestyle limiting hip pain, she was advised a total hip replacement surgery. She was made aware of the added risk of the surgery owing to atrial fibrillation and hypertension.


Preoperative X-ray images showing AP and frog-leg lateral view of the right hip
Risks, benefits, and alternatives including nonoperative and operative management were discussed in detail with the patient and her husband. She agreed to go ahead with the right total hip replacement. She was advised to get medical and cardiac clearance. She stopped Xarelto 3 days before the surgery.
OPERATION: Right total hip arthroplasty.
IMPLANTS USED: 52 mm cup with 6.5 mm screw, 25 mm in length with a 0-degree polyethylene with a 127-degree neck stem with a ceramic femoral head 36 mm minus 2.5.
DESCRIPTION OF PROCEDURE: The patient was brought to the operating room after obtaining informed consent, finding the correct surgical site. The risks, benefits, and alternatives were extensively discussed with the patient prior to the procedure. The patient was then definitively positioned in the lateral position after anesthesia and the right hip up was then draped and prepped in the usual sterile manner.
A curved incision centered over the greater trochanter was used for the arthrotomy. Skin and subcutaneous tissues were incised. The fascia was then divided. The hip was then placed into internal rotation and the posterior soft tissue structures were then taken down and then tagged for future repair. The hip was then dislocated. Lesser trochanter to the center measurement was taken.
Neck resection was made at the correct level. Attention was then turned towards the acetabulum. The remainder of the labrum was then debrided. The acetabulum was then sequentially reamed. The final shell was then placed into position in the correct abduction and anteversion. A screw was used for additional fixation. A poly was then placed over the shell and attention was then turned towards the femur.
The femur was then sequentially broached. The final broach was left into position. The trunnion and the head were then placed over the stem. Lesser trochanter distance was measured and was found to be correct. The hip was then relocated. Trialed for a physiological range of motion.
There was no impingement. The stability was good. The hip was then dislocated. The trial components were then removed. The final components were then placed into position. The hip was then reduced. Thorough irrigation was given. Posterior soft tissue structures were then tagged to the greater trochanter through transosseous tunnels. The fascia was closed with Vicryl and Ethibond.
Cutaneous tissues were closed with Vicryl. Subcutaneous tissues were closed With Vicryl. The skin was closed using skin staples. Sterile dressing was then applied over the wound. The patient was then transferred to the postoperative care unit in stable condition.

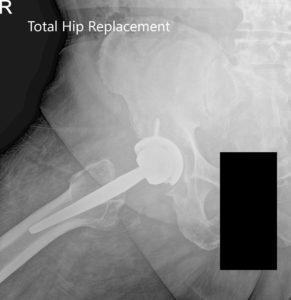
Postoperative X-ray showing AP and frog-leg lateral views of the right hip
Xarelto was resumed postoperatively and she was advised to use thrombo-embolic-deterrent (TED) stockings. She was allowed weight bearing as tolerated with support. The pain was well managed with medications. Skin staples were removed uneventful. She was advised gait training and fall prevention education was given to the patient.
She was compliant with hip precautions to prevent dislocation. Physical therapy was started to strengthen the muscles and increased flexibility. Three months into recovery, therapy and precautions, she was able to walk unaided pain-free. She was advised to gradually wean off hip precautions.
She was now happily back to her baseline activities and had resumed her routine of visiting the book club. She stated the results had exceeded all her expectations.

Dr. Suhirad Khokhar
My name is Dr. Suhirad Khokhar, and am an orthopaedic surgeon. I completed my MBBS (Bachelor of Medicine & Bachelor of Surgery) at Govt. Medical College, Patiala, India.
I specialize in musculoskeletal disorders and their management, and have personally approved of and written this content.
My profile page has all of my educational information, work experience, and all the pages on this site that I've contributed to.
