Case Study: Left Knee Arthroscopy: Medial Meniscectomy
and Abrasion Chondroplasty in a 51 year-old patient
Knee injuries entail damage to one or more of the ligaments, tendons, cartilage, bones, and muscles that make up the knee joint. These kinds of wounds can be brought on by a fall, a forceful knee twist, a car accident with significant impact, or another cause.
With the use of a surgical technique called a knee arthroscopy, doctors may inspect the knee joint without having to remove a significant amount of skin and soft tissue. Numerous knee issues can be identified and treated using arthroscopy.
A 51 year-old patient was in our office with complaints regarding left knee pain. She has been treated by Dr. Albert and got a cortisone injection. For aggravating factors, standing, walking, upstairs, and downstairs.
For associated symptoms, weakness, numbness, tingling, swelling, and radiation but reports no redness, no warmth, no ecchymosis, no catching/locking, no popping/clicking, no buckling, no grinding, no instability, no radiation, no fever, no chills, no weight loss, no change in bowel/bladder habits, and no tenderness.
The patient presented MRI results that showed moderate to markedly advanced patellofemoral compartment chondromalacia. Free edge fraying of the medial meniscus with an obliquely oriented undersurface horizontal flap tear through the body of the medial meniscus and mild to moderate generalized medial compartment chondromalacia.
Mild free edge fraying of the lateral meniscus without a discrete tear. Trace joint effusion with an 8mm ossified loose body at the posterior aspect of the joint.
MRI-3T Left knee non-contrast
We discussed the treatment options for the patient’s diagnosis, which included living with the extremity as it is, organized exercises, medicines, injections and surgical options. We also discussed the nature and purpose of the treatment options along with the expected risks and benefits.
I educated the patient regarding the inherent and unavoidable risks which include, but are not limited to anesthesia, infection, damage to nerves and blood vessels, blood loss, blood clots, and even death were discussed at length.
We also talked about the possibility of not being able to return to prior activities or employment, the need for future surgery, and complex regional pain syndrome. The patient also understands there is a long rehabilitative process that typically follows the surgical procedure.
We talked about the possibility of not being able to alleviate all of the discomfort. Also, I explained there is no guarantee all the function and strength will return. The patient also understands the risks of re-tear or failure to heal. The patient understands implants may be utilized during this surgery.
The patient expressed understanding of these risks and has elected to proceed with surgery. We have discussed the surgical procedure as well as the realistic expectations regarding the risks, outcome and post operative protocol.
The patient was taken to the operating room where she was placed on a well-padded operating table. Left lower extremity was prepped and draped tourniquet. Preop antibiotic was given. Time-out was called. Tourniquet was elevated after using Esmarch.
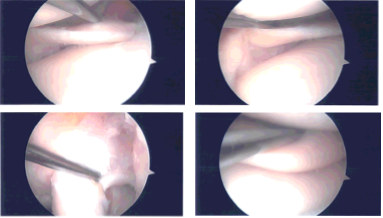
A lateral entry portal was made and arthroscope was inserted. A medial entry portal was made with the use of spinal needle. Examination of the knee showed arthritic changes in the medial femoral head as well as tearing of the medial meniscus along the anterior horn.
No tear could be found in the posterior horn, posterior root as well as posterior body of the medial meniscus.
Debridement of the medial meniscus of the anterior horn was performed with the use of shaver. Chondroplasty of the medial femoral condyle was also performed with the use of a shaver. Examination of the intercondylar notch showed intact ACL with degeneration.
Examination of the lateral compartment, tibiofemoral compartment showed intact lateral meniscus as well as bilateral tibiofemoral compartment. Examination of the patellofemoral compartment showed grade 3 to grade 4 osteoarthritis of the trochlea as well as inferior surface of patella.
Debridement of the patellofemoral joint was performed with the use of shaver. Abrasion chondroplasty was also performed with shaver along as well as the patella. Final pictures were taken for safety. The knee was thoroughly irrigated.
Intraoperative Arthroscopy Images
Closure was done with the use of # 3-0 nylon. A 40 mg of Depo-Medrol mixed with 9 cc of 0.5% Marcaine was injected into the knee. Dressing was done with the use of Xeroform, 4 x 8, Webril, and Ace wrap. The patient was extubated and moved to recovery in a stable condition.
The patient was seen for post operative check up. We have decided to do formal physical therapy as well as a home exercise program for rehabilitation of the knee.
The patient did well after the surgery and continued physical therapy. Patient checked in for a follow up visit after a month and saw significant improvement on her knee.
Disclaimer – Patient’s name, age, sex, dates, events have been changed or modified to protect patient privacy.
I am Vedant Vaksha, Fellowship trained Spine, Sports and Arthroscopic Surgeon at Complete Orthopedics. I take care of patients with ailments of the neck, back, shoulder, knee, elbow and ankle. I personally approve this content and have written most of it myself.
Please take a look at my profile page and don't hesitate to come in and talk.