Case Study: Management of ACL Tear
and Meniscal Injury in a 30-year-old Female
The patient is a 30-year-old female who is in our office after sustaining an injury to the right knee while playing soccer a week ago. The patient reports she sustained a twisting injury when her cleats got stuck. The patient reported pain and popping sound on sustaining the injury. The right knee swelling has decreased over the past week.
The patient reports sharp pain on the inner side of the right knee and a feeling of giving away while bearing weight. The patient has been using crutches following the injury. Activities such as walking, stairs, turning, twisting make the symptoms worse. Icing and rest make the symptoms better.
The patient previously reports the injury to the right knee twice in the past 5 years. She had a right knee full-thickness ACL tear a year and a half ago. She is currently on oral contraceptive pills and ibuprofen. She denies any history of smoking or use of illicit drugs. The reports no known drug allergies.
The physical examination of the right knee revealed patellar tap positive, tenderness at the medial joint line, anterior drawer test positive, Lachmann test positive, Apley’s maneuver positive, Mcmurray’s test positive for medial and lateral meniscus. The range of motion of restricted secondary to pain with flexion (80 deg), and extension (10 deg.).
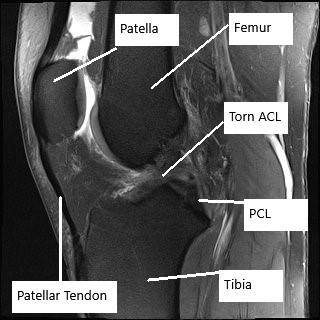
MRI of the knee in the sagittal section showing torn ACL.
MRI of the right knee revealed a full-thickness ACL tear with a bone contusion pattern indicative of a recent anterior tibial translation. The ACL tear has now progressed to full-thickness and is worse compared to the prior study. Tearing of the medial and lateral meniscus, progressive in severity since the prior study.
Various treatment options were discussed at length with the patient and the patient opted for surgical management. The risks and benefits including infection, bleeding, injury to adjacent nerves and vessels, stiffness, need for rehabilitation, the possibility of development of arthritis and early need for total knee replacement, systemic complications including blood clot, pulmonary, neurological, and cardiac complications including death were discussed at length. The patient understood and signed the informed consent.
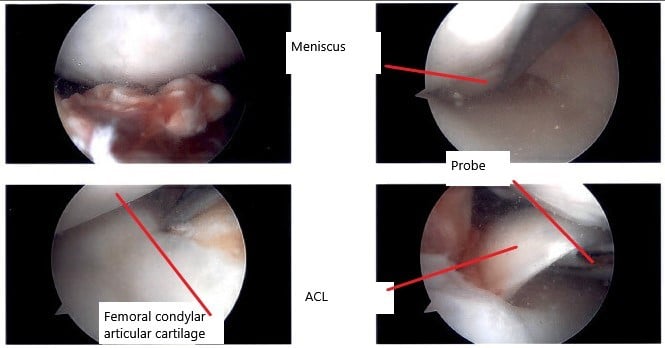
Intraoperative arthroscope image of the right knee.
PREOPERATIVE DIAGNOSES:
- Tear of the ACL, right knee.
- Tear of the medial meniscus, right knee.
- Tear of the lateral meniscus, right knee.
POSTOPERATIVE DIAGNOSES:
- Tear of the ACL, right knee.
- Tear of the medial meniscus, right knee.
- Tear of the lateral meniscus, right knee.
OPERATIONS:
- Right knee arthroscopic ACL reconstruction using quadriceps autograft.
- Right knee medial meniscectomy.
- Right knee lateral meniscectomy.
DESCRIPTION OF PROCEDURE: The patient was taken to the operating room and was placed on a well-padded operating table. General anesthesia was induced. The right lower extremity was prepped and draped aseptically after application of a tourniquet. The preop antibiotic was given. Time-out was called. Tourniquet was not inflated at this time.
Quadriceps tendon graft harvest was planned. A suprapatellar midline incision was given about 3 cm. With sharp dissection, the quadriceps tendon was reached. With blunt dissection, the quadriceps tendon would be dissected proximally along the lateral border of vastus medialis obliquus. It was checked and removed with the arthroscope. A 7 mm deep and 10 mm wide Arthrex preloaded blade was used to cut the graft, did a partial cut into the quadriceps tendon.
The tendon was cut with sharp dissection from over the superior port of the patella. The suture was passed into the distal quadriceps to have elevated. With sharp dissection, a partial-thickness quadriceps graft was elevated for about 80 mm. There was a rent in the capsule, which was sealed later on with #0 Vicryl.
The graft cutter was used to elevate the graft up to 80 mm and cut. The graft was removed and the capsule was sutured. The suprapatellar incision was packed with the Ray-Tec. The graft was prepared on the back table. Now, the tourniquet was elevated after the application of Esmarch.
The arthroscope was entered through the lateral entry portal. Examination of the patellofemoral compartment showed no arthritic changes. Examination of the medial patellofemoral compartment showed grade 3 to grade 4 change in a small patch over the medial femoral condyle. The meniscus showed an inferior flap over the posterior horn, which was removed with the shaver. There was no ramp lesion or meniscal tear. The scope was entered into the intercondylar notch where the ACL was found to be torn.
The ACL was debrided with the use of a shaver. The PCL was intact. The medial wall of the lateral femoral condyle was cleaned and debrided for identification of the footprint of the ACL. The tibial footprint of the ACL was also debrided. The arthroscope was entered into the lateral femoral condyle and lateral tibiofemoral compartment.
It showed grade 3 to grade 4 arthritic changes over a third of the femoral condyle. Also, there was a bad tear in the lateral meniscus, which was extending from the mid-body to the posterior body and the posterior horn across the popliteal hiatus.
The meniscus was not repairable. So, it was debrided with the use of shaver and biters. Balanced edges were obtained at the end of the meniscectomy. Debridement of the lateral femoral condyle was also performed. Now, a PassPort cannula was entered through the medial portal. Lateral femoral zig was used to make an entry canal for the femoral tunnel. A FlipCutter was used and a 25 mm canal was made using the FlipCutter in a usual fashion.
The bone shavings were debrided. Now, a tibial tunnel was made from the medial entry portal and a 20 mm tunnel was made in a similar fashion with the FlipCutter. The all-inside technique was utilized. The graft was passed through the suture lasso into the femoral and followed by the tibial tunnel. The graft was sutured using FiberTak and TightRope RT on either end. Either end was passed with the femoral and the tibial tunnel. The button was repeated on either side and tightened over the bony cortex.
After full tightening, the graft was tied in satisfactorily. The femoral side was tightened first. The tibial side was tightened and the knee cycled from flexion to extension 30 times. The button on the tibial side was not fully grounded. The SwiveLock was inserted distally through the tibial tunnel on the medial side after drilling and tapping.
The suture was encountered into the SwiveLock and inserted and tightened completely. Once the core suture of the SwiveLock was tied onto the TightRope and cut flush with the knots on either side. The wounds were thoroughly irrigated. The closure was done in layers using #0 Vicryl, #3-0 Monocryl, and #3-0 nylon.
Final arthroscopic pictures were taken and saved. Knee was dressed using 4 x 4, ABD, Webril, and Ace wrap. A knee immobilizer was applied. The patient was extubated and moved to recovery in a stable condition.
Disclaimer – Patient’s name, age, sex, dates, events have been changed or modified to protect patient privacy.

Dr. Suhirad Khokhar
My name is Dr. Suhirad Khokhar, and am an orthopaedic surgeon. I completed my MBBS (Bachelor of Medicine & Bachelor of Surgery) at Govt. Medical College, Patiala, India.
I specialize in musculoskeletal disorders and their management, and have personally approved of and written this content.
My profile page has all of my educational information, work experience, and all the pages on this site that I've contributed to.
